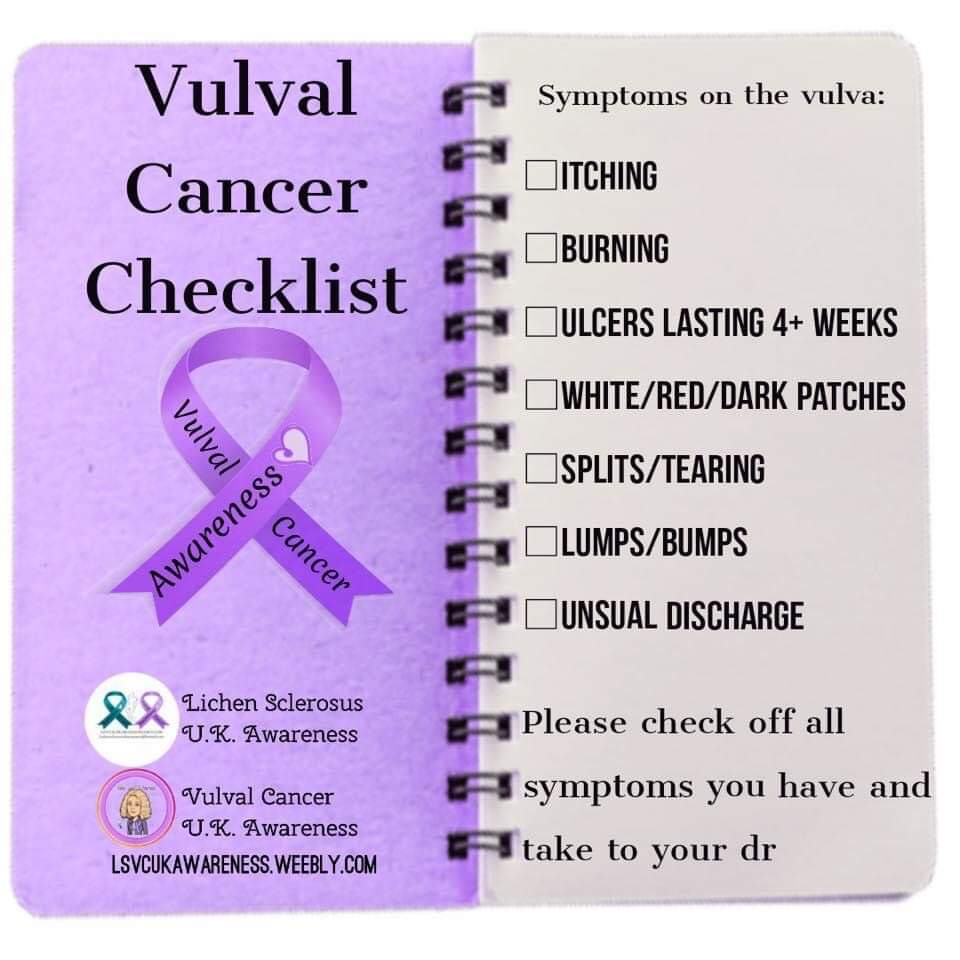
Symptoms of Vulval Cancer
Symptoms of vulval cancer can include:
An itch on the Vulva that persists.
Pain or soreness on the vulva
Raised and thickened patches of skin that can be red, white or dark.
A lump or wart looking growth on the vulva
Bleeding/open sores on the vulva or blood-stained vaginal discharge between periods
Burning when urinating.
A mole on the vulva that changes shape or colour.
An itch on the Vulva that persists.
Pain or soreness on the vulva
Raised and thickened patches of skin that can be red, white or dark.
A lump or wart looking growth on the vulva
Bleeding/open sores on the vulva or blood-stained vaginal discharge between periods
Burning when urinating.
A mole on the vulva that changes shape or colour.
Vulval Cancer Overview
Patients who have:
Lichen Sclerosus
Padgets
HPV
VIN
Differentiated VIN
CIN
Cervical Cancer
Lupus
Psoriasis
Radiotherapy for Womb Cancer
are at a higher risk of developing Vulval Cancer.
In 2015 it was found that there were 1339 new cases of Vulva cancer in the UK, 460 deaths of Vulva Cancer patients and 53% survived for 10 yrs or more. As with all cancers, early detection is the key to a successful treatment or prevention.
HPV is a factor in the development of some vulval cancers. Please see HPV section for more details on this.
It is important to know that most women infected with HPV do not go on to develop vulval cancer. For many people the virus causes no harm and goes away without treatment.
HPV type 16 is the most common type found in vulval cancer, followed by HPV types 33 and 18. Infection with these types of HPV types does not usually produce any warts or other visible signs until precancerous changes or cancer develop.
This is why it is so important to check for changes to your vulva every week as you would check your breasts. Get to know your Vulva and what is normal.
There is no need to feel embarrassed about going to your gp regarding any changes to your vulva! Thats what they are there for and will have seen thousands of Vulva's before seeing yours. This appointment could save your life.
Lichen Sclerosus
Padgets
HPV
VIN
Differentiated VIN
CIN
Cervical Cancer
Lupus
Psoriasis
Radiotherapy for Womb Cancer
are at a higher risk of developing Vulval Cancer.
In 2015 it was found that there were 1339 new cases of Vulva cancer in the UK, 460 deaths of Vulva Cancer patients and 53% survived for 10 yrs or more. As with all cancers, early detection is the key to a successful treatment or prevention.
HPV is a factor in the development of some vulval cancers. Please see HPV section for more details on this.
It is important to know that most women infected with HPV do not go on to develop vulval cancer. For many people the virus causes no harm and goes away without treatment.
HPV type 16 is the most common type found in vulval cancer, followed by HPV types 33 and 18. Infection with these types of HPV types does not usually produce any warts or other visible signs until precancerous changes or cancer develop.
This is why it is so important to check for changes to your vulva every week as you would check your breasts. Get to know your Vulva and what is normal.
There is no need to feel embarrassed about going to your gp regarding any changes to your vulva! Thats what they are there for and will have seen thousands of Vulva's before seeing yours. This appointment could save your life.
Eve Appeals research into Vulval Cancer
To help the Eve appeal Gynae cancer charity fund vital research into vulval cancer please use the donate button below, every little helps and will help to save womens lives.
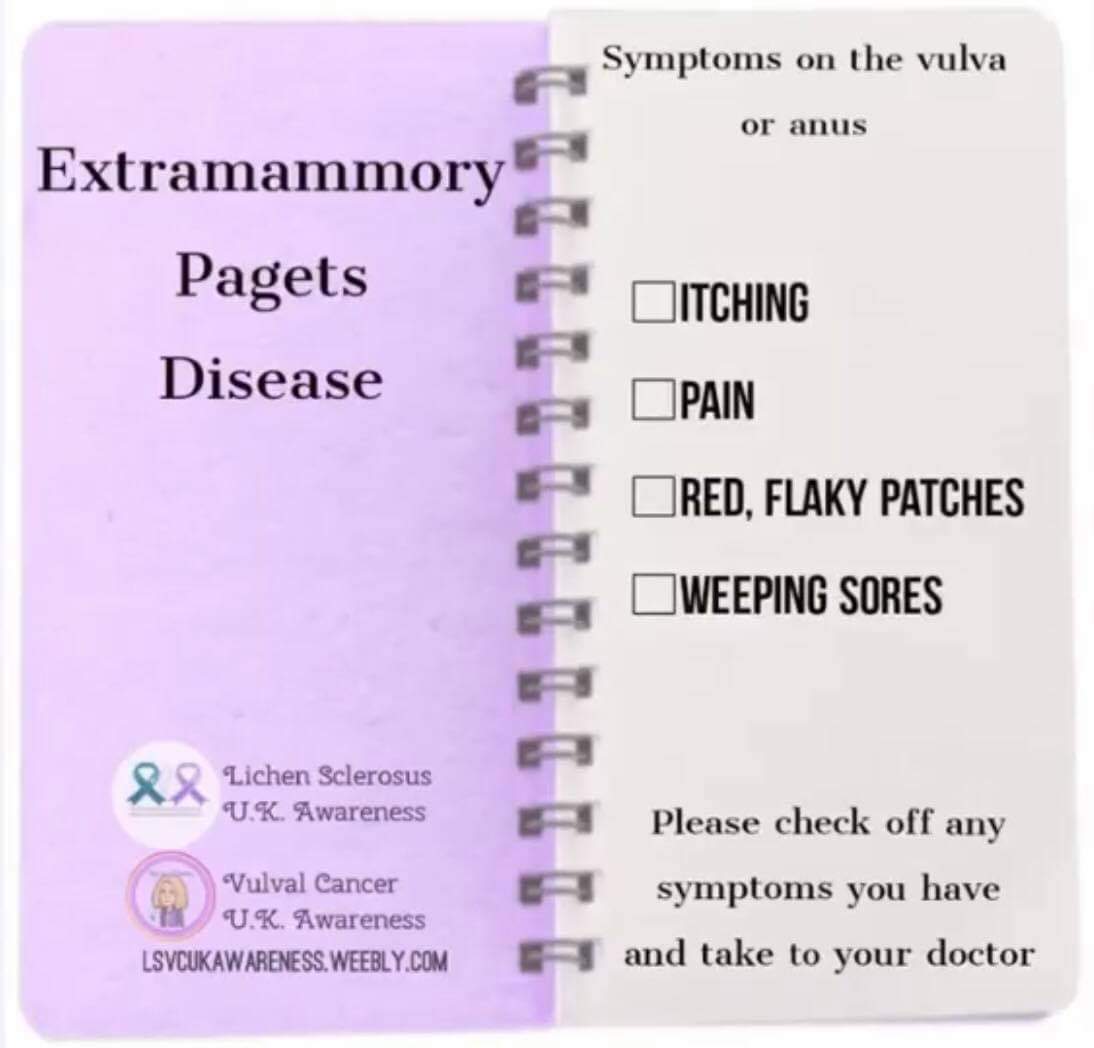
Extramammory padget's
Paget's is also called extramammary Paget's disease and affects both sexes, in the vulva, perineal or scrotal areas.
Paget’s disease of the vulva is a rare kind of skin cancer that arises from glandular cells. This disease appears as a red, velvety area with white patches on the vulva. It may also present as pink in colour, and occasionally there are moist, weeping ulcers that bleed easily. Most people with the condition will experience itching and soreness.
The cause of this disorder is unknown and is usually diagnosed by a biopsy. The typical treatment is surgery excision. The excision should be wide enough to get a disease-free margin, usually 1.5 to 2 cm away from the visible lesion. There is no need to remove the lymph nodes in the groin, if there is no invasion. In more severe cases, you may need to have skin grafting to close the wound. The tumor will frequently extend into what appears to be normal skin, making the extent of the surgical resection difficult to determine.
Approximately 15% of patients with vulvar Paget’s disease will also have invasive Paget’s disease or an underlying invasive adenocarcinoma of the vulva. You will need to be carefully followed and seen regularly by your doctor long term because this condition can frequently come back.
The prognosis for extramammary Paget disease (EMPD) depends on early diagnosis and surgical treatment. The prognosis is good for cases where the disease only affects the epidermal (top) layer of skin and the areas around the surgically removed lesion (margins) remain free of the disease. One study showed a mortality rate of 18% for patients without associated carcinoma and 46% for those with underlying carcinoma. Perianal disease, invasion into the dermal skin layer, and spread of cancer to lymph nodes are more likely to be associated with a poor prognosis. The rate of recurrence is approximately 30%. In those people who experience a recurrence of extramammary Paget disease, the average time it takes for the disease to recur is 2.5 years
High prevalence of low expression and hypermethylation of CDH1 gene was detected in 48% of cases, respectively which indicates a link to it being hereditary. Recurrence rates range between 30–60%.
Paget’s disease of the vulva is a rare kind of skin cancer that arises from glandular cells. This disease appears as a red, velvety area with white patches on the vulva. It may also present as pink in colour, and occasionally there are moist, weeping ulcers that bleed easily. Most people with the condition will experience itching and soreness.
The cause of this disorder is unknown and is usually diagnosed by a biopsy. The typical treatment is surgery excision. The excision should be wide enough to get a disease-free margin, usually 1.5 to 2 cm away from the visible lesion. There is no need to remove the lymph nodes in the groin, if there is no invasion. In more severe cases, you may need to have skin grafting to close the wound. The tumor will frequently extend into what appears to be normal skin, making the extent of the surgical resection difficult to determine.
Approximately 15% of patients with vulvar Paget’s disease will also have invasive Paget’s disease or an underlying invasive adenocarcinoma of the vulva. You will need to be carefully followed and seen regularly by your doctor long term because this condition can frequently come back.
The prognosis for extramammary Paget disease (EMPD) depends on early diagnosis and surgical treatment. The prognosis is good for cases where the disease only affects the epidermal (top) layer of skin and the areas around the surgically removed lesion (margins) remain free of the disease. One study showed a mortality rate of 18% for patients without associated carcinoma and 46% for those with underlying carcinoma. Perianal disease, invasion into the dermal skin layer, and spread of cancer to lymph nodes are more likely to be associated with a poor prognosis. The rate of recurrence is approximately 30%. In those people who experience a recurrence of extramammary Paget disease, the average time it takes for the disease to recur is 2.5 years
High prevalence of low expression and hypermethylation of CDH1 gene was detected in 48% of cases, respectively which indicates a link to it being hereditary. Recurrence rates range between 30–60%.