|
🎀 Gynecological Cancer Awareness Month
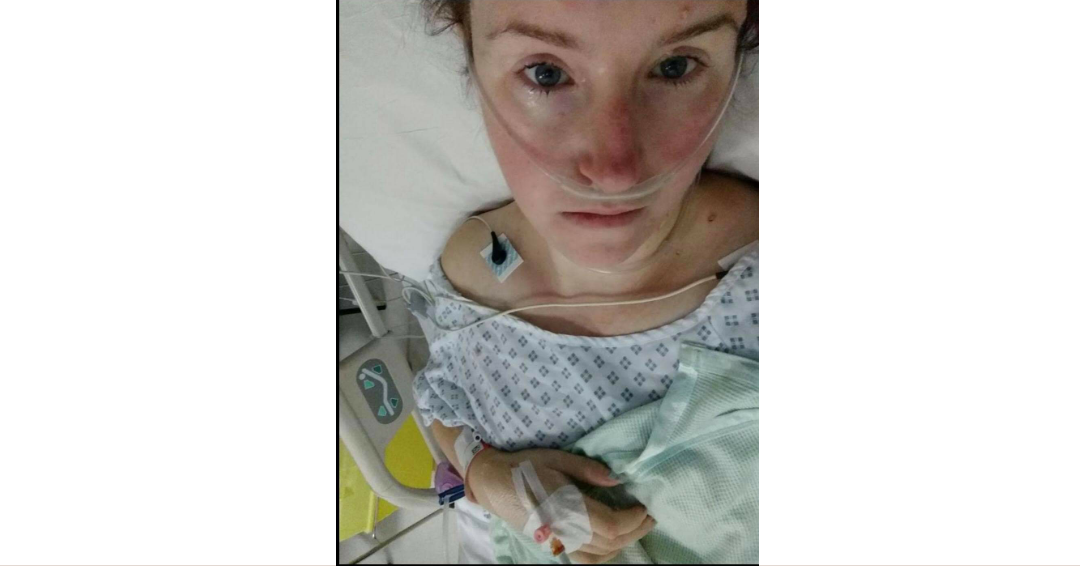
🎀 I wanted to do this post a lot earlier this month but if I'm completely honest, the memories are more painful than I'd like to admit, but that's okay, right? 🎀 Of all the Gynecological Cancers I'd heard of, Vulval Cancer was definitely off my radar when I realised they were concerned about the lump. 🎀I'd had 3 different cancers before,so I was vigilant of ANY changes but maybe a bit naive in thinking they could just cut it off couldn't they?! 🎀Wrong. The biopsy itself was one of the most painful things iv ever been through,I was drinking Oramorph like it was water,I just wanted the pain to stop. After confirming Squamous Cell Carcinoma,I was booked in for surgery,always a longer process for me personally as I already have several different health issues. 🎀 After coming round in ICU, I was so glad to see the doctor, she did an amazing job and got great margins, we'd already had a discussion about possibly having Radiotherapy because of where the tumour was and size (6cm) to see if they could zap the teeny tiny cells that were left over 🎀 12 weeks later,I had Radiotherapy at Christies, I found that harder than ANYTHING iv ever had to endure,I can only describe it like sitting on a barbecue for 25 days in a row...not pleasant. 🎀But it worked, like a dream and I'm here, because of those doctors and nurses. Don't put it off,they are specifically trained in that area and want to help. This is my story and if it helps someone else, i'll tell it all day! Everyday I have issues because of this treatment but I think myself lucky a million times over!!
0 Comments
Vulval Cancer – I had never heard of it, but I knew I had it.
When offered the opportunity to tell my story I immediately thought ‘YES, YES, YES - I have to tell the story of my journey with this horrible life changing disease. I have an obligation to do my bit to help the fight to get this cancer recognised and known about by ALL women of ALL ages, men, GP’s and all other Health care professionals. To stop the stigma surrounding the words ‘vulva’ or ‘vagina’ and start talking about this cancer in the same way we do others. I would also like to show all women that we know our body’s best and that we owe it to ourselves to know our normal in order to be our best advocates. When I was first diagnosed, I was determined that I wasn’t going to have a ‘journey’ or a ‘story’. I didn’t have anything against them, they were just ‘not my thing’. How naïve was I? I have since reflected on this and realised that at that point I was angry. Everybody has a journey or a story, whatever you wish to call it. Life itself is our own personal story. I knew long before I was diagnosed that this is what it was. I was angry that I was fobbed off more than once by professionals, treated for something it wasn’t, and made to feel like I am ‘exaggerating’ the excruciating pain I was constantly in. So, here goes. Here is my story. I am Nicky Beresford. Married to my husband Matt for 8 years now and we have been together for 10 years. We have a beautiful 6 year old boy named Fletcher. It was around April 2019 that I first noticed some small red spots on my vulva. They were uncomfortable, however, as a lot of us women do, I ignored it as I was training to run my first ever half marathon for Alzheimer’s disease. My Dad was living with it and I was determined to do something for him to raise awareness for this disease. I told myself that it was probably just friction from running or something. As the weeks went on the pain was getting increasingly worse and I noticed the area affected was getting bigger and I knew this wasn’t right. I only had a week to go before the half marathon. I made an appointment with my GP for early June and lathered my vulva up with lidocaine (Vagisil) to help ease some of the pain. I ran the half and finished! On my first visit to the GP, I had hardly even started to describe my symptoms when she turned immediately to her VDU and uttered the words ‘Oh, you shouldn’t be here, you should be at the sexual health clinic, we don’t deal with these things here’. She immediately made me feel worthless and that I was wasting her time, I was absolutely floored. No one should be made to feel that way by a GP. I somehow uttered some words to her to try and explain that I didn’t think it was anything sexual health related and I think I need to be examined. She responded by telling me the local clinic had a drop in centre that morning and that I should go there for care. She hasn’t even examined me at this point. I insisted that I should be examined. She reluctantly agreed, although it was clear that she had already made her mind up. She took one quick look and said ‘yes, you shouldn’t be here, you need to go to the sexual health drop in.’ I left the GP’s office and phoned my husband in tears. I did what I was told and I went to the drop in. I was seen by a lovely Dr who asked me lots of questions about my health and history. She was very kind and understanding and followed with a full examination. She immediately told me that she wasn’t sure what this was, but that it didn’t look to be a sexual health condition. She took swabs and blood tests to do a full sexual health screening. She asked me to go back when I had had all the results back. As anticipated, my test results all came back clear, but as instructed I went back to see her. We were now in early July and the pain was getting increasingly worse and the area affected seemed to be getting bigger. She went through all of my tests, and on re-examination she advised me to go back to my GP for a second opinion and said I may need to be referred to a dermatologist. So, I got back into the car, rang my husband to tell him and then immediately rang my GP to get another appointment. It was with another GP as I didn’t feel comfortable going back to the previous one. I had hoped I may have a better experience. The appointment was another 3 weeks away. The pain was getting worse by the day and I noticed a small red lump had formed on the top of my clitoris. I was now using lidocaine on a daily basis (Matt and I joked that I should have shares in the stuff as I couldn’t leave the house without ensuring I had plenty with me). I was also finding that it was stinging when I went for a wee. It was becoming uncomfortable to sit, walk and wear trousers. I was not sleeping, my mood was low, and I was struggling more and more each day. Then the day came – appointment day! I was so sure that I would be taken seriously now and that I would be referred. I was called through to the GP’s room. I sat down, poured my heart out about everything that had happened and what I was experiencing. He simply said to me ‘It sounds like you have Lichen Sclerosus and some steroids will sort it out’. I had never heard of it but he said it was a skin condition. Amazingly, this GP didn’t even examine me and said he didn’t need to. He diagnosed me just like that! I explained that the Dr at sexual health had said I should be referred to a dermatologist. I was sent away to see how the cream helped at first. I went home in floods of tears. Over the next few weeks the pain was increasingly unbearable and going to the toilet was horrific. One day I broke down in tears at work and had to leave. I got home and my husband just held me and said ‘enough is enough, we are going private’. We didn’t have the funds to go private as we were saving to move house and have a bigger mortgage. But, he insisted. I got an appointment within a day with a consultant who specialised in gynaecological skin conditions. He couldn’t have been nicer if he tried. He could see the pain in my face and as soon as he examined me he could see why. He prescribed some different steroid cream as he saw that there may be some kind of skin infection, but wanted to see me again in a weeks’ time for a closer examination when this had calmed down. Unfortunately this clashed with a weekend away for my little boy’s birthday to Legoland, which was a surprise for his 5th Birthday. We talked about how to manage the pain and that to give me some relief the best thing would be to wear skirts and no knickers as much as possible. He also prescribed me some thick dermal aqueous cream to act as a barrier when going to the loo. I had at least felt listened to at last and an appointment was made for when we got back from Legoland. I spent the weekend away in agony, constantly applying lidocaine and this thick cream to try and ease the excruciating pain. And if any of my colleagues read this, yes, I spent the last 4 months of 2019 at work with no knickers on! I attended my follow up, and some of the inflammation had gone down but the Dr was really concerned about the size of the red lesions, the thickening of the skin and growth on my clitoris – not to mention the increasing pain I was in. I hit the ceiling when he attempted to examine me. He immediately referred me to his colleague, for a second opinion. I saw her the very next evening. She immediately took one look at my vulva and with concern she sat me down and said that before she could be certain, she would need me to have biopsies taken, but this could be something called VIN (Vulval intraepithel neoplasia). There was no way I could afford to pay for biopsies to be taken privately. I panicked, but she assured me she would speak to her colleague at the local NHS gynaecological department at Leighton Hospital and request an urgent referral. I got home and immediately started googling VIN and other gynaecological skin conditions and all sorts of things came up. Yes, I know I shouldn’t rely on google but on extensive searching of articles and images, I knew this was vulval cancer. I just knew. I had a call 2 days later and was asked to go in for biopsies to be taken the following week. I thought the pain I was in enough, but having someone taking a punch biopsy from the most sensitive part of your body that is already painful beyond belief is crucifying! Think of a Dr with a tiny apple corer removing pieces of your skin! I think I almost stopped the blood flow in the nurses’ hand I was holding and the words ‘potty mouthed’ doesn’t come close to the language coming out of my mouth. Now I had to wait for the results. 2 excruciating weeks! The results were in. The consultant sat me down and she had a look that I knew meant it wasn’t good news. I did Have VIN. VIN Stage 3. I had read about this, these are abnormal cells in the top layer of the epidermis and the level 1, 2 or 3 is how deep into the skin they go. This was followed by telling me I am being referred to the Christie Cancer Hospital in Manchester as they don’t have the specialists required to deal with this condition. All I heard was ‘Christie and Cancer’. I received the referral letter and my appointment was the 1st week of January in 2020. We were mid-October by this point. Week by week, life was increasingly difficult. The area affected was getting harder and harder to deal with, I was getting no relief and I literally had to scream if I wanted to have a wee. It got to the point in early December where I just couldn’t take it anymore. It was constant. This resulted in me having a total breakdown in work. I had no idea how I would get through Christmas. I sought help from an urgent care centre who prescribed me some tramadol to help ease the pain. She also prescribed more lidocaine which no longer provided the slightest bit of relief. I felt like every day the red legions were getting bigger and the growth on my clitoris was getting bigger. I was so miserable by this point. The tramadol didn’t seem to help much, so with Christmas a couple of days away now, I got a last minute appointment to see the nurse practitioner at my local GP surgery. I simply broke down to her and said that I cannot take the pain any more. I told her the story, she saw my notes and she prescribed me some morphine to take alongside the tramadol. She also gave me some anaesthetic gel to apply directly onto my vulva to try and help. Like many professionals, she wasn’t familiar with the condition, but she was kind and could see how much I was struggling and did her best to help me. Christmas was a blur, but we managed to make it a good one – I think! Morphine, tramadol and gin helped! January couldn’t come quick enough for me. The day arrived and I am sat in the consultant’s room at The Christie. He examined me and he couldn’t even touch me without me squealing and edging away. He asked me to get dressed and come and sit back down. The words that came next were a shock, but at the same time, they weren’t. He said that he can see the incredible amount of pain I was in and on looking at my vulva, in his experience we are looking at vulval cancer. He went onto explain that I would need to go in to have a general anaesthetic so that they could take several deeper biopsies to confirm this, but that I should also prepare myself that the tumour over the clitoris is so large that it may be difficult to save it, and that it is likely that I will lose it altogether. I just looked at the nurse and said ‘I have a little boy’. I was numb. My husband was numb. We kind of knew this was coming, but nothing prepares you for hearing those words. I am lucky as I have ‘THE’ best husband in the world. He took me into his arms and said ‘hey, it’s me and you and you know that together we can get through anything, and we WILL get through this’. The biopsies confirmed that it was vulval cancer the day before we moved house. My oncologist advised that I would have surgery to remove the cancer which would consist of an anterior vulvectomy including the excision of the clitoris, with bilateral sentinel lymph node removal of the groin. I would also have to attend the nuclear medicine department for sentinel node location and imaging on the morning of the surgery. Surgery was set for the 17th February 2020. This imaging consisted of injecting a radioactive dye right into the heart of the lesions and the pain, to identify the nodes and it filled me with complete fear. At least I would be asleep for the bulk of the surgery. I had been in pain for so long that it didn’t matter anymore. I could hardly walk as it was due to the pain, what was a few more seconds? My husband heard the screams from the waiting room – but it was over quickly. Just the surgery to get through now. I woke up after the surgery. I had tubes coming out of me, a drip, a catheter and I was hooked up to all sorts of machines bleeping away. I was in a ward full of other women, with various types of cancers and who had undergone various types of surgery. All with stories of their own. It saddened me listening to their stories, but their humour and warmth filled me with such positivity. I felt lucky that I had come through the surgery and it was likely that radiotherapy or chemotherapy was not going to be necessary if my lymph nodes are clear. Later that night, the lights went down and the patients tried to sleep. That was when I was alone with my thoughts. What audience did I have to raise awareness? Did I want the world to know what I have? What I have had done? I mean, it’s my ‘private bits’ (the ones we are not allowed to talk about). So I did it. I wrote the hardest FB post I have ever had to write. I told all of my FB friends and acquaintances. I needed them to hear it, as like most of us diagnosed with it, it’s unknown and it’s often diagnosed later than it should be and that scares me as women are suffering. If just one person heard my story, and it made a difference to them, or allowed one woman to go and see a Dr about a concern. Then it would be worth it. As hard as it was, I received so much love and support and several women and a few chaps private messaged me and thanked me for sharing it. The following morning, I had the catheter taken out and the nurse asked me to go to the toilet and wee into the cardboard bowl. I couldn’t do it. I had been having a wee with the catheter in, so didn’t have the pain that I was in before. I simply couldn’t have a wee as I was petrified of the pain I would once again feel. A lovely nurse could see how distressed I was, and came with me to help me have a wee. It’s at this point where you have a total respect for what these marvellous humans do. She made me laugh and gave me the courage to just ‘let it flow’. So I did. It was marvellous and it was ‘PAIN FREE’. It was the best wee I have ever had! It had been so painful for so long that I had forgotten what it was like to have a pain free wee. Getting over the surgery was long and hard. The swelling, the pain, the daily injections and wearing the ever so lovely compression stockings was uncomfortable. Sleeping was difficult and I am a very impatient patient! I knew that I had a long journey ahead just to heal and that’s before I even started thinking about the long term impact. Then the Coronavirus lockdown happened. The trips to The Christie were difficult and I had to go unaccompanied, with my husband and son having to drop me off and wait for me. The Christie was always busy, but always had a positive buzz about it. Now, it was deserted, almost eerie. Everyone in masks and visors, temperatures and history checked on arrival. It was a very different place. On a positive note, the cancer hadn’t spread through my lymph nodes. Following on and to reduce the numbers in the hospital, some of my check up’s were done via the telephone and that was when I was told that I needed more surgery. The multi-disciplinary team had discussed my results and although they were confident they had got all of the cancer, the margins were not as clear as they would like. In order to reduce the likelihood of it returning, I needed to have more surgery. I was just starting to get back to a bit more normality after surgery, so this came as a blow. I was set back and although I knew it was a possibility, I had convinced myself it wouldn’t be necessary. The weekend before my surgery was due to take place, I developed an infection in my groin on the left hand side starting at the wounds where they had taken my lymph nodes. This spread rapidly across my pubis and was excruciating. Another trip to the consult confirmed it as cellulitis and I was given 2 lots of antibiotics and my surgery was postponed. It took over 2 weeks for the infection to clear. Once I had received the all clear from the consultant I was told that the surgery would be rescheduled, however with Covid, they were unable to give me a timeframe. I felt like I was living with a time bomb and that the longer I had to wait, the more the cancer could grow back. I think I must have been a nightmare to live with during this time. Surgery was scheduled for the 1st June 2020. I wasn’t allowed to have anyone to accompany me, so I had to go in to the hospital on my own. This was particularly hard, as sometimes, no matter how old you are, you need someone to hold your hand and give you the strength you need. Surgery went well. It was not as traumatic as last time. I was sore and swollen again and I had lots of bed rest ahead of me, more daily injections (to reduce blood clots) and more surgical stockings. I was fed up, sad, angry and I struggled to see the positives as it hit home hard that my body will never be the same again. The questions wouldn’t stop spinning around in my head. How do I even begin to have a physical relationship again with my husband? Will our marriage survive this? How will I face people at work? Will I always be known as ‘the Mum at school who had vulval cancer’? And the most frightening is - what if it comes back again? But there is one huge positive. I am here to be a Mummy to my little boy. I am also here to be able to share my story and hope to prevent other women going through such trauma. I also hope I can help to spread the word about this cancer and support the incredible work that the Vulval Cancer UK support group founder is doing to raise awareness and get people talking about this. Whatever age you are, talk to your daughters, your wife, your Mum, Aunty, Sister and know your own normal. Don’t put off going to the GP, no matter how busy your life is. Be your own body advocate, you know it better than anyone else. My journey is not over, but life is getting back on track and day by day and I am learning to live with my ‘new normal’. It won’t happen overnight, but I am back at work, I have restarted my running, and life is slowly returning to something similar to what it was before. I didn’t ask for cancer, no one does. But, if I can take one positive from this awful time, it is to cherish your life, no matter how tough it may be at the time. Be kind to yourself and be kind to each other. Oh, and CHECK your VULVA! Nicky x In about 2006 I went to my gp for my routine smear test. The nurse asked me if I had noticed anything unusual. I replied no. She says she will take a swab in case I have an infection. She also tells me that my skin is very white.
My smear test came back that I needed testing again. Redone the test and all was fine. Now my gp decided to refer me to the dermatology dept at the hospital. I was seen by a dermatologist and a gynaecologist. Here I start on the beginning of a long road. My very first punch biopsies, they were brutal. Results came back lichen sclerosus. Ointments and creams are prescribed and followed to religiously. Now I am in the hospital outpatient rotation. Started with every three to four months. The first punch biopsy hadn't healed. Months of going back and forth changing creams and ointments. Seeing different doctors. They would talk of doing more biopsies. The second and the third bled on the fourth they offered to bring me in to get it done under a general. To be honest even though it hurts getting them done, the healing afterwards is off the scale with pain. I could hardly walk, sit, lie or even sleep. So I bite the bullet and get them done as an outpatient. Four years of hospital appointments it is decided LS. I should just carry on using the ointments. I have been taken off from outpatients Here followed the next couple of years of using the prescription dermovate cream as directed. I even searched the Internet for help. I came across silver nitrate cream, which I tried. I was even prescribed dermasilk medical pants. Which were suppose to soothe and heal. They were to be worn 24/7 no need for creams. I found that they didn't help. So went back to use using dermovate. My vulva was angry red and ulcerated. Bleeding at the merest touch of toilet paper. I built up courage to go back and share my problem with my gp. I went back to my doctor and she took one look and did an urgent referral to gynae. Even at that point I didn't think it was serious. Got my 7th punch biopsy, consultant called me back to outpatients, where we discussed an inscission to cut the ulcer out, that was November 2018. As I had a bowel prolapse both operations were scheduled together. February 2019 i had both operations. My gynae consultant and I chatted as I was getting ready to go home. I remember him saying "the biopsy was sent for testing and as far as he could see everything was fine" Less than a week later I had a phone call, could I come in to discuss the results. I knew then, even when he told me it was Cancer I asked well what do we do next? Next thing I had was a CT scan which showed that there was no sign of any suspicious cells. Followed by a MDT meeting. My gynae consulted with a consultant oncologist where they thought it wise to offer me a bilateral groin lymph node dissection. On meeting the oncologist, we discussed the operation or whether to wait and see. I chose the operation. It was a 90% chance they would be clear. In June 2019 I had the lymph nodes removed. The results were clear. A side effect was cellulitis in my groin and hips. My oncologist has prescribed me a daily dose of low dosage penicillin as preventative medicine. I also have lymphodema and have compression tights, these are a great help. 2020, I phoned my Cnc with concerns with changes on my vulva. At the end of February the gynae consultant saw me at a clinic. I had a white cauliflower growth on my clitoris area. He decide it would be better to remove it. March 2020 I had my pre-med for operation at the beginning of April. Covid-19 was very prevelent then and my surgery was cancelled. So back to watch and wait. I contacted the hospital again as now the growth is weeping and changed size and colour. Gynae see's changes and has arranged my surgery again. Due to be carried out on the 8th September. Then the growth will be sent off to the lab. God knows what next. But I will try to live, love and laugh |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
August 2023
Categories |


 RSS Feed
RSS Feed
