|
I'm a guy of 41 years old and I was diagnosed with lichen sclerosus about 3 years ago.
It took a long time for the actual diagnosis because I was told it was because I wasn't washing and that it may be an STI. At the time I was in a long term relationship. It caused arguments over cheating but obviously that didn't happen. The dermatologist was a woman to my relief as I did ask for a female because I don't do well with other males. There was no sense of dignity at the first appointment. I was told to strip from the waist down, there where 4 women in the room. After the dermatologist checked my penis she asked for pictures. One of the nurses started to take pictures of my penis with the foreskin pulled back. They didn't explain why and I started to get upset and started crying. They stopped and asked if I was OK. I explained why I got upset and I had to sign a form of consent for the pictures to be taken. I was given an appointment for a biopsy, I asked for it to be female only because of what I previously explained. They were more than happy to oblige. (I was sexually abused and raped by both males and females from the age of 4. I'm scared of males because it was only them that hurt me) On the day of the biopsy the 2 female staff were really nice and understood why I was so scared. They both explained what was happening every step of the way My penis was made numb by injection, they checked it was numb then took a biopsy from the corona and put stitches in. They were both very professional and my dignity was taken into consideration. After a week the stitches were removed and again my dignity was considered as there was a young female trainee there, she was asked to leave while the stitches were removed. At the appointment I was told it was LS and it was explained to me in detail which I was grateful of since the last appointment there was so upsetting. Over the past year my LS has gotten worse. I suffer from erectile dysfunction due to my mental health and testicular pain caused by nerve damage from an operation to remove a varicocele at the age of 19. Getting an erection is painful not just in my testicles but now in my penis because the foreskin has fused to the corona to the point you can't see the corona or ridge etc. If I try to have sex I just bleed as it splits. Due to my sexual problems, my mental health and a recent diagnosis of autism (no learning disabilities) my partner of 17 years split with me and had been cheating on me due to my problems. It hit hard and I ended up in a mental health hospital due to being on the wrong side of a bridge. Thankfully I'm still here and I now only live for the sake of my 2 children because they are all I have left in life. Lately my LS is getting a lot worse and it hurts to have a wee. I have difficulty anyway and have to sit down because it takes about 15 mins for me to start to wee because of some of my medication. The foreskin slits a lot from the glands penis and bleeds heavily. Its very embarrassing when I'm at work and have to ask the female supervisor for a sanitary towel. (She knows my problems but it's still embarrassing). The glands penis is very painful and frequently I get a lot of white spots because of the LS. I've been waiting for nearly a year for a new appointment with no sign of it coming anytime soon. Last time the dermatologist said I may need a circumcision and a full glands resurfacing. It's not really what I want but only if I have no other choice. I'm scared to death of an operation due to the last operation I had on my genitals, it went badly wrong and caused the nerve pain which never goes away and sometimes when so bad it feels like I've been kicked in the balls and I can't walk or anything. I'm also scared because there is a family history of penile cancer. My grandad had penile cancer and had to have his whole penis removed then it spread and his testicles, prostate and bladder which were removed. Sadly it still spread and it took his life. Due to the Lichen sclerosus, the family history of penile cancer and the fact this has caused the break up of my 17 year relationship, I'm living a nightmare where I just can't wake up from and I'm scared to death. One last thing, I know absolutely nobody male or female who has LS. I've no support, nobody who I can speak to and have understanding. I feel so alone in it all.
2 Comments
I had always imagined I’d write a book or at least a chapter about my work in early years education, not about the ongoing relationship I have with my intimate skin conditions. In my twenties I accepted my lack of fertility and constant misdiagnosed bouts of thrush. Having a pinhole cervix, fibroids and endometriosis didn’t bode well and after numerous years of suffering and trialing different treatment, monthly Zoladex implants and key hole surgery to establish the extent of disease, I ended up having a full hysterectomy. You get used to being uncomfortable and begin to label it as such, rather than acknowledging it as pain. But after a couple of years after my op I suddenly experienced a normality, no bloating, no heavy bleeding and no pain! However, the continuing whiteness and uncomfortable vulva continued, with sex becoming increasingly painful. I recall being away on holiday when my GP phoned to tell me to stop using the pessaries I had been prescribed for thrush, as my swabs had come back negative, she was unsure what was wrong. They did every STD test they could but still drew a blank. I was living away from home for a while and with a new GP when they decided to undertake exploratory keyhole surgery prior to my hysterectomy. It was at this point that I was first diagnosed with a chronic skin condition of my vulva, Lichen Sclerosus. I was sent away with Dermovate the strongest topical steroid they prescribe and told to apply if I become sore. No other information, monitoring or advice! I kept up the steroid when I felt it was needed but also tried alternatives, but to no avail! Then as I approached my five decade year I noticed a spot on my labia that didn’t heal with the steroid, got bigger and became ulcerated. My GP referred me back to gynae and although being told I’d been seen within six weeks, there was no need to worry, so after a five month wait I was finally seen and sent straight away for a biopsy of my vulva. Within two weeks I was told my LS had developed into pre cancerous cells of a high grade, dVIN. So on my fiftieth birthday I headed for my pre op, having being reassured they had caught it early and a WLE to rid me of the nasty invaders was the way forward. The surgery was pretty brutal as they had spotted a bigger area that they needed to investigate. Nine days later hubby and I sat in a very small quiet waiting room, awaiting the results to say I had vulva cancer! On reflection from that point to six months after my hemi vulvectomy and removal of groin lymph nodes, is all quite a blur! I was fortunate to stumble across the LS and VC Facebook support groups, which helped me understand and process all I was going through. Now three years on I thought that was the end of my story but no it’s a continuing journey. I was diagnosed with vulva Lichen Planus, on top of LS, surgery has caused me to suffer with pubic lymphedema, which means I have to massage daily, balance the length of time I sit still or exercise and I have physio for damage surgery caused to my nerves and ligaments. I did mange six months of being in control of the LS & LP but my recent gynae oncology review has informed me that the LS is in a flare up, the LP is beginning to travel in to my vagina and there is another area that will be reviewed in a month. I’m an up beat and confident woman but these silent invaders wreak havoc with my emotional wellness. It took a while, due to the pandemic, to access counselling and it is something I have definitely needed. Theses experiences change you, a cancer diagnosis throws it’s own issues into the mix and although I’m extremely grateful I was naive to think I would return to a life without issues. Yes I’m lucky to have amazing family and friends but I have changed and don’t often like to show how I’m feeling as I now feel it’s a burden, it’s boring or it comes across as me being negative, even depressed! Rationalising this negativity comes and goes, a clumsy comment can trigger a stress trauma which I can find hard to deal with. There is also the huge effort and expense of the required self care; products, clothing and feeling of self indulgence for needing to ‘find’ time to undertake all the self care. I don’t write to scare or worry others but to highlight the constant need to defend our rights, to shine a light on the need for awareness and to get through those dark days. It is an invisible ghost that haunts my sleep and thoughts in a way I could never have predicted. I have to accept although compliant with all my treatments, it’s incurable and won’t leave me alone! I try hard to enjoy every moment and not allow it to take control of me, even though deep down the anxiety can be hard to hide. So what I have learnt is to know your body, fight hard to be heard and be seen as only you know what is going on, nobody else walks your path or shares your pain. Be bold, be brave be true to you! X I was 28 when I was diagnosed with lichen sclerosis. My son was 9 months old when I started to get symptoms. After several trips to the GP and being told it was allergic reactions and thrush I saw a new GP with an interest in women’s health. She diagnosed me immediately and started me on a steroid regime, I saw an improvement very quickly and was put on 6 monthly visits to a dermatologist.
I was terrified of the diagnosis and the google searches didn’t help that. I suffer from health anxiety and the last thing someone like me needs is a condition with a raised risk of developing cancer. It’s something for the anxiety to feed off. I found myself constantly checking myself and becoming sore as a result which then panicked me more and it became a constant cycle. One thing that terrified me was the changes to my anatomy. Things looked and felt different, but then I would question if they had always been that way. I didn’t ever check before diagnosis and I certainly didn’t use a mirror to look at myself! I wondered if I’d always looked that way and what my “normal” actually was! I have had some fusing and I would be worried about everything disappearing,’I felt like every time I looked another part of me had gone. Soon I started to wonder about when I wanted another baby. I knew I wanted another but I thought it would no longer be an option and that made me feel awful. Intimacy had changed and the thought of having to try and conceive was scary. I hit a low point then and put a lot of pressure and blame on myself thinking I’d be responsible for us not having another child. In the end it wasn’t as scary or impossible as I thought. I got pregnant and I was lucky that my symptoms improved massively during pregnancy. My consultant reassured me that I could continue to use my steroid cream as I needed to. However at this point I found alternatives to help me along and used almond oil quite a bit, even with the reassurance I was worried I would do damage and, naturally, google throws up some worrying results when I looked at steroid use in pregnancy. I still had the odd flare up, something I put down to the hormones but i could manage, my biggest challenge was trying to do my regular examinations with a massive bowling ball bump in the way! Because of my diagnosis I decided to push for a c-section. I was all geared up for a battle when I went to meet my consultant but I really needn’t be! She was fantastic and said she had read up on the condition and was happy to go down either route with me supporting me the whole way. Having the c-section helped me to prepare for the birth, it took away the worries of labour for me. After the birth of my daughter my symptoms inevitably flared up again. Because of my hormones I struggled to settle them down, and having to remember the steroid with a newborn and a young son were also a challenge! I also worried about steroid use when breastfeeding. I spoke to my consultant and pharmacist and they told me the benefits outweighed the risks. I think however that was one of the reasons my symptoms took a while to settle, i didn’t use as much as I would pre-birth. I also developed anxiety post-natally which, oddly, was a bit of a blessing in disguise. I was referred for CBT and that helped me to address some of my health anxiety which in turn helped me with my LS. I am currently in a period of calm with my symptoms, I know when things are flaring up, I restrict my checks to regular periods of time and I know how to manage flare ups. I also try to speak about LS a little more. I’m not so great at doing it face to face but when possible I encourage women to “know they’re normal” and know when to look for help. I’m also determine to make sure my daughter (and son) know about this condition as well. To continue to raise awareness with the next generation. To say that being diagnosed with cancer is bloody scary would be a gross\nunderstatement. It’s like being hit in the head with a hammer and\nsimultaneously being kicked in the nuts, although in this case it might be more\nfitting to describe it as a kick in the uterus!
\n\nI was first alerted to something being wrong in late summer of 2018 when my\nperiods got very painful. \n\nHowever, this wasn’t the first change to my periods: about 18 months or so\nbefore I went to the doctor, my periods had been getting heavier and longer.\nBut these changes were gradual, and I put them down to my age and changes in\nhormonal balance. I thought maybe I was heading towards an early menopause,\nespecially as I occasionally used to get what I thought were hot flushes. I\nknow better now that I have experienced what real hot flushes are like. I also\nnow know that any changes to periods, gradual or not, can be a sign of womb\ncancer. But I had no idea then. \n\nThe pain prompted me to see a doctor. There are several doctors who work at\nmy GP and I chose the one who specialises in women’s health. I’d heard stories\nof doctors not looking deeper into the causes of changes to periods but just\nprescribing the pill or a coil, and I thought that perhaps someone specialised\nin the field would be more likely to investigate the cause. \n\nI was right. She said before we decide what to do about the long and heavy\nperiods, she would refer me to a gynaecologist. In the meantime, she prescribed\nme medication to help with the pain and heavy bleeding. They didn’t work. What\nworked best for me at this point were painkillers called Feminax Express.\nNormal painkillers worked, too, but I had to take more of them as they were not\nas strong. \n\nFrom the initial appointment with my GP, it took nearly three months for my\ngynaecologist appointment in which they could tell that I had a thickened\nlining in my womb. Since they couldn’t tell more from this examination, they\nreferred me for a hysteroscopy. This time I had to wait about a month for the\nappointment by which time my periods had got even longer and I was having pain\neven when I wasn’t bleeding. I was having to take pain killers every day. \n\nDuring the hysteroscopy, the gynaecologist took a biopsy, and then we waited\nagain. Not so long this time, though. When it was time to get my results, I\nasked my partner Justin to come with me. Initially, I was going to go alone to\nthe appointment to get the results, but I had a gut feeling that I would not\nlike the news. I’m so bloody glad Justin came with me. \n\nThe moment my doctor mentioned the word cancer, I could think of nothing\nelse. The word bounced around my brain, leaving no space for anything else\nexcept: I can’t have cancer! I don’t want to die! Because, let’s face it, we\nstill associate the disease with death despite the progress made in treating\nit. \n\nEventually I focused on what he was telling me again: I would need to have a\nhysterectomy and possibly further treatment after the surgery. OK, hysterectomy\nI could handle, especially as after I got home I Googled uterine cancer and to\nmy delight read that hysterectomy is often the only treatment needed to remove\nthe disease. For now, I’d focus on getting through the surgery and then deal\nwith the rest. Hoping that there wouldn’t be ‘the rest’ to deal with. \n\nWhen I got home, I had to make the hardest phone calls ever to tell my\nfamily what was going on. How do you tell your parents and your sister and\nbrother that you have cancer? I’m afraid I was quite blunt; I just blurted it\nout. But then, I was crying from the word go, so they knew something was wrong\nstraight away. And what made it harder was that all my family is still in\nFinland (I moved here 25 years ago) and during times like this you want your\nfamily close. \n\nThey were ready to come over whenever needed and my sister came over for a\nfew days before the surgery and my parents when I got out of the hospital. And\nof course, I had my partner by my side the entire time! \n\nI still can’t believe how quickly everything proceeded after the diagnosis.\nIn less than two weeks after seeing my doctor, I was getting ready for the\nsurgery. I was, as everyone would be, nervous about the surgery but knew that I\nhad an excellent, experienced surgeon specialised in oncology. He, and all the\nother staff at St George’s Hospital in Tooting, were nothing short of amazing. \n\nThe dedication, the positivity and the care of all the staff throughout my\nstay at the hospital was incredible. It made me fully realise how lucky I am to\nlive in a country with free health care and such amazingly devoted nurses and\ndoctors. \n\nWhen my surgeon came to see me he explained that he had done a long cut from\nunderneath the naval to nearly my breastbone to remove the tumour and all the\ninfected lymph nodes. I was in a such a drowsy state that it wasn’t until a\ncouple of days later when he came to see me again that I fully understood the\nextent of the surgery. No wonder every move I made hurt like hell! \n\nMy surgery was on a Friday and they let me go home on Monday since I could\nget to the toilet on my own and my bladder and bowels worked ok. I lost count\nof how many times they asked me about my bowel movements. \n\nMy hopes of hysterectomy being the end of the treatments crashed when I saw\nmy surgeon two weeks after the operation. He is amazing at what he does in the\noperating theatre, but his people skills are not on par. \n\nEven though he mentioned again that the operation went well and they got the\ndisease out, he then launched into an explanation of how my cancer was of a\nrare, aggressive type more commonly seen in women over sixty. Then dropped the\nother C-bomb: chemotherapy. \n\nHe told me I would need several courses of chemo followed by radiation. It\ndidn’t make matters any better that he would not give me a clear prognosis;\ninstead he said something about it being hard to tell whether I would be in the\none-in-ten group that make it. He said he’d know more after I’d gone through\nthe chemo and radiotherapies. \n\nNot surprisingly, I thought there was only a 10 percent chance of surviving.\nThe thoughts of death I’d had after the initial diagnosis made a quick\ncomeback. \n\nMy opinion of his communication skills did not improve when, a few weeks\nlater, I received a copy of a letter he had sent to my GP. In that he mentioned\nthat the patient, that being me, became very upset during the appointment. Too\nright I did! Who wouldn’t when being told they have a very aggressive, rare\ncancer! I bet there would not be many who could receive that news with a stiff\nupper lip and a poker face. \n\nLuckily, I also met the oncologist who was going to be in charge of my\nchemotherapy and radiation treatments at the Royal Marsden in Chelsea. I have\nsince discovered that she is the Head of Clinical Oncology at Royal Marsden, so\nI couldn’t have been in better hands. She made me feel better and more hopeful. \n\nShe emphasised the fact that the operation had gone very well and there were\nno signs of disease left. She also explained that the purpose of the therapy\nwas to prevent the tumour from coming back or metastasising. Because she emphasised\nthat there was no visual evidence of the cancer, I could leave the hospital\nfeeling more positive. \n\nMy six courses of chemo weren’t too bad. I lost my hair and had trouble with\nlow platelet counts, but other than that I did not have serious side-effects.\nRadiotherapy got me harder. The fatigue that hit me after about ten sessions of\nradiotherapy was nothing I had experienced before. However much I rested and\nslept, I was still constantly tired. It has taken months to rebuild my energy\nlevels, but I’m getting there. \n\nMy experience has left me with the desire to spread awareness of womb cancer\nso that more women would know to see a doctor earlier than I did. Had I known\nthe symptoms, I would have known to see my doctor sooner and the cancer would\nnot have had the chance to spread outside the womb. When womb cancer is\ndiagnosed at stage one, the survival rate is around 90-95% depending on the\nsource. At stage three, the rate drops to about 50%. So early diagnosis, like\nwith all cancers, saves lives. \n\nThe main symptom of womb cancer is abnormal vaginal bleeding. This includes\nany changes to periods or bleeding between periods. It also includes any\nvaginal bleeding after menopause. \n\nSymptoms other than abnormal bleeding can include: \n\n- watery or bloody vaginal discharge \n\n- long lasting bloated or swollen tummy \n\n- feeling full quickly or loss of appetite \n\n- pain in the lower tummy or pelvis most of the time \n\n- peeing more often than usual or more urgently \n\n- diarrhoea or constipation \n\n- back pain \n\n- feeling tired all the time \n\nRemember, having any of these symptoms, even abnormal vaginal bleeding,\ndoesn’t mean that you definitely have womb cancer. However, you should always\nhave abnormal bleeding investigated. \n\nYou can read more about my experiences in my blog Cycling for Cancer\n(https://cyclingforcancer.co.uk/ ). You’ll also be able to follow our (my\npartner and I) preparation for an epic cycle ride across Europe in Agust 2021\nto raise money for the Royal Marsden Cancer Charity. 🎀 Gynecological Cancer Awareness Month
🎀 I wanted to do this post a lot earlier this month but if I'm completely honest, the memories are more painful than I'd like to admit, but that's okay, right? 🎀 Of all the Gynecological Cancers I'd heard of, Vulval Cancer was definitely off my radar when I realised they were concerned about the lump. 🎀I'd had 3 different cancers before,so I was vigilant of ANY changes but maybe a bit naive in thinking they could just cut it off couldn't they?! 🎀Wrong. The biopsy itself was one of the most painful things iv ever been through,I was drinking Oramorph like it was water,I just wanted the pain to stop. After confirming Squamous Cell Carcinoma,I was booked in for surgery,always a longer process for me personally as I already have several different health issues. 🎀 After coming round in ICU, I was so glad to see the doctor, she did an amazing job and got great margins, we'd already had a discussion about possibly having Radiotherapy because of where the tumour was and size (6cm) to see if they could zap the teeny tiny cells that were left over 🎀 12 weeks later,I had Radiotherapy at Christies, I found that harder than ANYTHING iv ever had to endure,I can only describe it like sitting on a barbecue for 25 days in a row...not pleasant. 🎀But it worked, like a dream and I'm here, because of those doctors and nurses. Don't put it off,they are specifically trained in that area and want to help. This is my story and if it helps someone else, i'll tell it all day! Everyday I have issues because of this treatment but I think myself lucky a million times over!! Vulval Cancer – I had never heard of it, but I knew I had it.
When offered the opportunity to tell my story I immediately thought ‘YES, YES, YES - I have to tell the story of my journey with this horrible life changing disease. I have an obligation to do my bit to help the fight to get this cancer recognised and known about by ALL women of ALL ages, men, GP’s and all other Health care professionals. To stop the stigma surrounding the words ‘vulva’ or ‘vagina’ and start talking about this cancer in the same way we do others. I would also like to show all women that we know our body’s best and that we owe it to ourselves to know our normal in order to be our best advocates. When I was first diagnosed, I was determined that I wasn’t going to have a ‘journey’ or a ‘story’. I didn’t have anything against them, they were just ‘not my thing’. How naïve was I? I have since reflected on this and realised that at that point I was angry. Everybody has a journey or a story, whatever you wish to call it. Life itself is our own personal story. I knew long before I was diagnosed that this is what it was. I was angry that I was fobbed off more than once by professionals, treated for something it wasn’t, and made to feel like I am ‘exaggerating’ the excruciating pain I was constantly in. So, here goes. Here is my story. I am Nicky Beresford. Married to my husband Matt for 8 years now and we have been together for 10 years. We have a beautiful 6 year old boy named Fletcher. It was around April 2019 that I first noticed some small red spots on my vulva. They were uncomfortable, however, as a lot of us women do, I ignored it as I was training to run my first ever half marathon for Alzheimer’s disease. My Dad was living with it and I was determined to do something for him to raise awareness for this disease. I told myself that it was probably just friction from running or something. As the weeks went on the pain was getting increasingly worse and I noticed the area affected was getting bigger and I knew this wasn’t right. I only had a week to go before the half marathon. I made an appointment with my GP for early June and lathered my vulva up with lidocaine (Vagisil) to help ease some of the pain. I ran the half and finished! On my first visit to the GP, I had hardly even started to describe my symptoms when she turned immediately to her VDU and uttered the words ‘Oh, you shouldn’t be here, you should be at the sexual health clinic, we don’t deal with these things here’. She immediately made me feel worthless and that I was wasting her time, I was absolutely floored. No one should be made to feel that way by a GP. I somehow uttered some words to her to try and explain that I didn’t think it was anything sexual health related and I think I need to be examined. She responded by telling me the local clinic had a drop in centre that morning and that I should go there for care. She hasn’t even examined me at this point. I insisted that I should be examined. She reluctantly agreed, although it was clear that she had already made her mind up. She took one quick look and said ‘yes, you shouldn’t be here, you need to go to the sexual health drop in.’ I left the GP’s office and phoned my husband in tears. I did what I was told and I went to the drop in. I was seen by a lovely Dr who asked me lots of questions about my health and history. She was very kind and understanding and followed with a full examination. She immediately told me that she wasn’t sure what this was, but that it didn’t look to be a sexual health condition. She took swabs and blood tests to do a full sexual health screening. She asked me to go back when I had had all the results back. As anticipated, my test results all came back clear, but as instructed I went back to see her. We were now in early July and the pain was getting increasingly worse and the area affected seemed to be getting bigger. She went through all of my tests, and on re-examination she advised me to go back to my GP for a second opinion and said I may need to be referred to a dermatologist. So, I got back into the car, rang my husband to tell him and then immediately rang my GP to get another appointment. It was with another GP as I didn’t feel comfortable going back to the previous one. I had hoped I may have a better experience. The appointment was another 3 weeks away. The pain was getting worse by the day and I noticed a small red lump had formed on the top of my clitoris. I was now using lidocaine on a daily basis (Matt and I joked that I should have shares in the stuff as I couldn’t leave the house without ensuring I had plenty with me). I was also finding that it was stinging when I went for a wee. It was becoming uncomfortable to sit, walk and wear trousers. I was not sleeping, my mood was low, and I was struggling more and more each day. Then the day came – appointment day! I was so sure that I would be taken seriously now and that I would be referred. I was called through to the GP’s room. I sat down, poured my heart out about everything that had happened and what I was experiencing. He simply said to me ‘It sounds like you have Lichen Sclerosus and some steroids will sort it out’. I had never heard of it but he said it was a skin condition. Amazingly, this GP didn’t even examine me and said he didn’t need to. He diagnosed me just like that! I explained that the Dr at sexual health had said I should be referred to a dermatologist. I was sent away to see how the cream helped at first. I went home in floods of tears. Over the next few weeks the pain was increasingly unbearable and going to the toilet was horrific. One day I broke down in tears at work and had to leave. I got home and my husband just held me and said ‘enough is enough, we are going private’. We didn’t have the funds to go private as we were saving to move house and have a bigger mortgage. But, he insisted. I got an appointment within a day with a consultant who specialised in gynaecological skin conditions. He couldn’t have been nicer if he tried. He could see the pain in my face and as soon as he examined me he could see why. He prescribed some different steroid cream as he saw that there may be some kind of skin infection, but wanted to see me again in a weeks’ time for a closer examination when this had calmed down. Unfortunately this clashed with a weekend away for my little boy’s birthday to Legoland, which was a surprise for his 5th Birthday. We talked about how to manage the pain and that to give me some relief the best thing would be to wear skirts and no knickers as much as possible. He also prescribed me some thick dermal aqueous cream to act as a barrier when going to the loo. I had at least felt listened to at last and an appointment was made for when we got back from Legoland. I spent the weekend away in agony, constantly applying lidocaine and this thick cream to try and ease the excruciating pain. And if any of my colleagues read this, yes, I spent the last 4 months of 2019 at work with no knickers on! I attended my follow up, and some of the inflammation had gone down but the Dr was really concerned about the size of the red lesions, the thickening of the skin and growth on my clitoris – not to mention the increasing pain I was in. I hit the ceiling when he attempted to examine me. He immediately referred me to his colleague, for a second opinion. I saw her the very next evening. She immediately took one look at my vulva and with concern she sat me down and said that before she could be certain, she would need me to have biopsies taken, but this could be something called VIN (Vulval intraepithel neoplasia). There was no way I could afford to pay for biopsies to be taken privately. I panicked, but she assured me she would speak to her colleague at the local NHS gynaecological department at Leighton Hospital and request an urgent referral. I got home and immediately started googling VIN and other gynaecological skin conditions and all sorts of things came up. Yes, I know I shouldn’t rely on google but on extensive searching of articles and images, I knew this was vulval cancer. I just knew. I had a call 2 days later and was asked to go in for biopsies to be taken the following week. I thought the pain I was in enough, but having someone taking a punch biopsy from the most sensitive part of your body that is already painful beyond belief is crucifying! Think of a Dr with a tiny apple corer removing pieces of your skin! I think I almost stopped the blood flow in the nurses’ hand I was holding and the words ‘potty mouthed’ doesn’t come close to the language coming out of my mouth. Now I had to wait for the results. 2 excruciating weeks! The results were in. The consultant sat me down and she had a look that I knew meant it wasn’t good news. I did Have VIN. VIN Stage 3. I had read about this, these are abnormal cells in the top layer of the epidermis and the level 1, 2 or 3 is how deep into the skin they go. This was followed by telling me I am being referred to the Christie Cancer Hospital in Manchester as they don’t have the specialists required to deal with this condition. All I heard was ‘Christie and Cancer’. I received the referral letter and my appointment was the 1st week of January in 2020. We were mid-October by this point. Week by week, life was increasingly difficult. The area affected was getting harder and harder to deal with, I was getting no relief and I literally had to scream if I wanted to have a wee. It got to the point in early December where I just couldn’t take it anymore. It was constant. This resulted in me having a total breakdown in work. I had no idea how I would get through Christmas. I sought help from an urgent care centre who prescribed me some tramadol to help ease the pain. She also prescribed more lidocaine which no longer provided the slightest bit of relief. I felt like every day the red legions were getting bigger and the growth on my clitoris was getting bigger. I was so miserable by this point. The tramadol didn’t seem to help much, so with Christmas a couple of days away now, I got a last minute appointment to see the nurse practitioner at my local GP surgery. I simply broke down to her and said that I cannot take the pain any more. I told her the story, she saw my notes and she prescribed me some morphine to take alongside the tramadol. She also gave me some anaesthetic gel to apply directly onto my vulva to try and help. Like many professionals, she wasn’t familiar with the condition, but she was kind and could see how much I was struggling and did her best to help me. Christmas was a blur, but we managed to make it a good one – I think! Morphine, tramadol and gin helped! January couldn’t come quick enough for me. The day arrived and I am sat in the consultant’s room at The Christie. He examined me and he couldn’t even touch me without me squealing and edging away. He asked me to get dressed and come and sit back down. The words that came next were a shock, but at the same time, they weren’t. He said that he can see the incredible amount of pain I was in and on looking at my vulva, in his experience we are looking at vulval cancer. He went onto explain that I would need to go in to have a general anaesthetic so that they could take several deeper biopsies to confirm this, but that I should also prepare myself that the tumour over the clitoris is so large that it may be difficult to save it, and that it is likely that I will lose it altogether. I just looked at the nurse and said ‘I have a little boy’. I was numb. My husband was numb. We kind of knew this was coming, but nothing prepares you for hearing those words. I am lucky as I have ‘THE’ best husband in the world. He took me into his arms and said ‘hey, it’s me and you and you know that together we can get through anything, and we WILL get through this’. The biopsies confirmed that it was vulval cancer the day before we moved house. My oncologist advised that I would have surgery to remove the cancer which would consist of an anterior vulvectomy including the excision of the clitoris, with bilateral sentinel lymph node removal of the groin. I would also have to attend the nuclear medicine department for sentinel node location and imaging on the morning of the surgery. Surgery was set for the 17th February 2020. This imaging consisted of injecting a radioactive dye right into the heart of the lesions and the pain, to identify the nodes and it filled me with complete fear. At least I would be asleep for the bulk of the surgery. I had been in pain for so long that it didn’t matter anymore. I could hardly walk as it was due to the pain, what was a few more seconds? My husband heard the screams from the waiting room – but it was over quickly. Just the surgery to get through now. I woke up after the surgery. I had tubes coming out of me, a drip, a catheter and I was hooked up to all sorts of machines bleeping away. I was in a ward full of other women, with various types of cancers and who had undergone various types of surgery. All with stories of their own. It saddened me listening to their stories, but their humour and warmth filled me with such positivity. I felt lucky that I had come through the surgery and it was likely that radiotherapy or chemotherapy was not going to be necessary if my lymph nodes are clear. Later that night, the lights went down and the patients tried to sleep. That was when I was alone with my thoughts. What audience did I have to raise awareness? Did I want the world to know what I have? What I have had done? I mean, it’s my ‘private bits’ (the ones we are not allowed to talk about). So I did it. I wrote the hardest FB post I have ever had to write. I told all of my FB friends and acquaintances. I needed them to hear it, as like most of us diagnosed with it, it’s unknown and it’s often diagnosed later than it should be and that scares me as women are suffering. If just one person heard my story, and it made a difference to them, or allowed one woman to go and see a Dr about a concern. Then it would be worth it. As hard as it was, I received so much love and support and several women and a few chaps private messaged me and thanked me for sharing it. The following morning, I had the catheter taken out and the nurse asked me to go to the toilet and wee into the cardboard bowl. I couldn’t do it. I had been having a wee with the catheter in, so didn’t have the pain that I was in before. I simply couldn’t have a wee as I was petrified of the pain I would once again feel. A lovely nurse could see how distressed I was, and came with me to help me have a wee. It’s at this point where you have a total respect for what these marvellous humans do. She made me laugh and gave me the courage to just ‘let it flow’. So I did. It was marvellous and it was ‘PAIN FREE’. It was the best wee I have ever had! It had been so painful for so long that I had forgotten what it was like to have a pain free wee. Getting over the surgery was long and hard. The swelling, the pain, the daily injections and wearing the ever so lovely compression stockings was uncomfortable. Sleeping was difficult and I am a very impatient patient! I knew that I had a long journey ahead just to heal and that’s before I even started thinking about the long term impact. Then the Coronavirus lockdown happened. The trips to The Christie were difficult and I had to go unaccompanied, with my husband and son having to drop me off and wait for me. The Christie was always busy, but always had a positive buzz about it. Now, it was deserted, almost eerie. Everyone in masks and visors, temperatures and history checked on arrival. It was a very different place. On a positive note, the cancer hadn’t spread through my lymph nodes. Following on and to reduce the numbers in the hospital, some of my check up’s were done via the telephone and that was when I was told that I needed more surgery. The multi-disciplinary team had discussed my results and although they were confident they had got all of the cancer, the margins were not as clear as they would like. In order to reduce the likelihood of it returning, I needed to have more surgery. I was just starting to get back to a bit more normality after surgery, so this came as a blow. I was set back and although I knew it was a possibility, I had convinced myself it wouldn’t be necessary. The weekend before my surgery was due to take place, I developed an infection in my groin on the left hand side starting at the wounds where they had taken my lymph nodes. This spread rapidly across my pubis and was excruciating. Another trip to the consult confirmed it as cellulitis and I was given 2 lots of antibiotics and my surgery was postponed. It took over 2 weeks for the infection to clear. Once I had received the all clear from the consultant I was told that the surgery would be rescheduled, however with Covid, they were unable to give me a timeframe. I felt like I was living with a time bomb and that the longer I had to wait, the more the cancer could grow back. I think I must have been a nightmare to live with during this time. Surgery was scheduled for the 1st June 2020. I wasn’t allowed to have anyone to accompany me, so I had to go in to the hospital on my own. This was particularly hard, as sometimes, no matter how old you are, you need someone to hold your hand and give you the strength you need. Surgery went well. It was not as traumatic as last time. I was sore and swollen again and I had lots of bed rest ahead of me, more daily injections (to reduce blood clots) and more surgical stockings. I was fed up, sad, angry and I struggled to see the positives as it hit home hard that my body will never be the same again. The questions wouldn’t stop spinning around in my head. How do I even begin to have a physical relationship again with my husband? Will our marriage survive this? How will I face people at work? Will I always be known as ‘the Mum at school who had vulval cancer’? And the most frightening is - what if it comes back again? But there is one huge positive. I am here to be a Mummy to my little boy. I am also here to be able to share my story and hope to prevent other women going through such trauma. I also hope I can help to spread the word about this cancer and support the incredible work that the Vulval Cancer UK support group founder is doing to raise awareness and get people talking about this. Whatever age you are, talk to your daughters, your wife, your Mum, Aunty, Sister and know your own normal. Don’t put off going to the GP, no matter how busy your life is. Be your own body advocate, you know it better than anyone else. My journey is not over, but life is getting back on track and day by day and I am learning to live with my ‘new normal’. It won’t happen overnight, but I am back at work, I have restarted my running, and life is slowly returning to something similar to what it was before. I didn’t ask for cancer, no one does. But, if I can take one positive from this awful time, it is to cherish your life, no matter how tough it may be at the time. Be kind to yourself and be kind to each other. Oh, and CHECK your VULVA! Nicky x In about 2006 I went to my gp for my routine smear test. The nurse asked me if I had noticed anything unusual. I replied no. She says she will take a swab in case I have an infection. She also tells me that my skin is very white.
My smear test came back that I needed testing again. Redone the test and all was fine. Now my gp decided to refer me to the dermatology dept at the hospital. I was seen by a dermatologist and a gynaecologist. Here I start on the beginning of a long road. My very first punch biopsies, they were brutal. Results came back lichen sclerosus. Ointments and creams are prescribed and followed to religiously. Now I am in the hospital outpatient rotation. Started with every three to four months. The first punch biopsy hadn't healed. Months of going back and forth changing creams and ointments. Seeing different doctors. They would talk of doing more biopsies. The second and the third bled on the fourth they offered to bring me in to get it done under a general. To be honest even though it hurts getting them done, the healing afterwards is off the scale with pain. I could hardly walk, sit, lie or even sleep. So I bite the bullet and get them done as an outpatient. Four years of hospital appointments it is decided LS. I should just carry on using the ointments. I have been taken off from outpatients Here followed the next couple of years of using the prescription dermovate cream as directed. I even searched the Internet for help. I came across silver nitrate cream, which I tried. I was even prescribed dermasilk medical pants. Which were suppose to soothe and heal. They were to be worn 24/7 no need for creams. I found that they didn't help. So went back to use using dermovate. My vulva was angry red and ulcerated. Bleeding at the merest touch of toilet paper. I built up courage to go back and share my problem with my gp. I went back to my doctor and she took one look and did an urgent referral to gynae. Even at that point I didn't think it was serious. Got my 7th punch biopsy, consultant called me back to outpatients, where we discussed an inscission to cut the ulcer out, that was November 2018. As I had a bowel prolapse both operations were scheduled together. February 2019 i had both operations. My gynae consultant and I chatted as I was getting ready to go home. I remember him saying "the biopsy was sent for testing and as far as he could see everything was fine" Less than a week later I had a phone call, could I come in to discuss the results. I knew then, even when he told me it was Cancer I asked well what do we do next? Next thing I had was a CT scan which showed that there was no sign of any suspicious cells. Followed by a MDT meeting. My gynae consulted with a consultant oncologist where they thought it wise to offer me a bilateral groin lymph node dissection. On meeting the oncologist, we discussed the operation or whether to wait and see. I chose the operation. It was a 90% chance they would be clear. In June 2019 I had the lymph nodes removed. The results were clear. A side effect was cellulitis in my groin and hips. My oncologist has prescribed me a daily dose of low dosage penicillin as preventative medicine. I also have lymphodema and have compression tights, these are a great help. 2020, I phoned my Cnc with concerns with changes on my vulva. At the end of February the gynae consultant saw me at a clinic. I had a white cauliflower growth on my clitoris area. He decide it would be better to remove it. March 2020 I had my pre-med for operation at the beginning of April. Covid-19 was very prevelent then and my surgery was cancelled. So back to watch and wait. I contacted the hospital again as now the growth is weeping and changed size and colour. Gynae see's changes and has arranged my surgery again. Due to be carried out on the 8th September. Then the growth will be sent off to the lab. God knows what next. But I will try to live, love and laugh We all do it, time speeds by and before I knew it, in the space of two years, I was married, and had two different jobs in the same organisation, always with a feeling of something isn’t quite right ‘down there’. By down there, I am of course referring to the vulva area which is the external female genital area, not to be confused (as it often is) with the internal areas which include the vagina, cervix, uterus and ovaries. During this time I had also had a cervical smear and thought, ‘Well if something is wrong, the nurse will flag it to me’ after all they see the external area when performing this test. This didn’t happen, so I wrongly put my concerns to the back of my mind as life took hold…fast forward a couple of years to April 2020.
No one predicted what 2020 would be like, least me and at the start of the year my main focus was looking forward to 40th birthday celebrations to be held at the end of the year. I didn’t think that I would be working from home on a day-to-day basis due to Covid 19 and my work would change focus to support the response to Covid 19. Neither did I know that this would be the opportunity for me to seek some advice about my increasing concern about ‘down below’, knowing that I was exhibiting some symptoms which were a real change for me including soreness, cracking and bleeding, which I noticed particularly when I walked. I’m guessing exacerbated by continuing to squeeze into a pair of skinny jeans. So mid April, I sheepishly made an appointment with a female GP, who called me to talk through the issue and then the horror struck me…she asked; ‘have you had a look at it’, to which I replied ashamedly, ‘no’. How embarrassing I thought to myself, not to look, not to check my own body. On reflection I can put that down to a few things, being busy, being ignorant or actually just a little bit scared to face into it, maybe a bit of all of the above?! The GP of course took this in her stride, after all I’m sure I’m not the first and certainly won’t be the last…unfortunately. So the task in hand, to hold up the mirror, which included a compact mirror and almost yoga like positions to see and immediately had that sinking feeling that something is really not right. The GP had already stated that she would call me back a couple of hours later, when she did and on the basis of what I found, a raw area with white plaque that I should come on in to be ‘eyeballed’. A couple of days later I went in to the GP surgery, after a very funny conversation in which it was agreed ‘no talking, we’ve already done that, just get your kit off’ to which I responded ‘no date?’ which lightened the issue. The GP was quick to act, saying she hadn’t seen anything like it before and off she referred me on the 2-week cancer pathway. I am very grateful the GP was quick, straightforward and honest. So two weeks on, I found myself at the local hospital, which during lockdown was a very strange place to be, primarily due to knowing generally only those people on the 2-week pathway or with cancer were being seen at this point during lockdown. The consultant again quick to act and mentioned ‘it looks like it’s VIN’…thinking to myself, I had not heard of this condition before, what is VIN?!. Immediately the consultant confirmed that I would need surgery and also warned me it would be highly likely to return. He gave me the option to have the biopsies there and then (best to get it out the way I thought’ and I actually said the words ‘yep, crack on’, laughing to myself afterwards, which was a welcome distraction as the biopsy procedure ensued. I did think prior to the appointment I’d more than likely be having biopsies, but hadn’t quite realised the extent to which I would be cut and stitched up, so the challenge was on to get home prior to the local anaesthetic wearing off, which was easy enough as the roads were quiet. Although I was uncomfortable down below, I was psychologically comfortable knowing that I would hear soon what I was facing for sure. Waiting is and uncertainty is hard, no way of dressing this up, it’s HARD and you hold on to the dates as target milestones, thinking you’re getting closer to getting sorted and knowing what the crack is (sorry another pun!). I received a letter asking me to go in about a month later for a ‘photo opportunity’. This provided some amusement to me and was being done to seek advice from the specialist in another hospital. I was told during this consultation that I was VIN2&3, however there was a strong chance there are ‘pinheads’ of cancer. I rationalised this in that the biopsies are only small areas taken away, so actually until it’s removed complete and the full histology has been completed you continue to not know for sure. Hearing the word cancer made me revert to a complete introvert and as a result I left without asking all the questions I needed to. Come July and I had been transferred from the local trust over to the nearest University Hospital. By now, I’m used to ‘the dreaded examination’ and now under the care of one of the leading consultants in vulvar disease in this country, for which I am very grateful. I am more grateful for the several opportunities the consultant enabled me to ask questions, which is a massive help and helps you form the questions you need to ask when you are on processing overload. I have received what I would describe as ‘all round care’, which I’d liken to a warm hug of support (social distanced of course!) from the hospitals Specialist Gynaecology oncology nurses. I’m now scheduled to have the wide local excision operation in early September and my next hurdle is to hope for clear margins. My op date also coincides with Gynaecological Awareness Month, which prompted me to share my experience to date. So this gets me thinking, ‘awareness’ what does this mean to me dealing with an issue, what do I think it should mean for every woman who hasn’t an issue? When I think about it, it’s really very basic, don’t be shy to hold up the mirror, do this regularly (once a month) and get to know your ‘normal’ or more importantly what isn’t normal and act on it. I spent far too much time thinking/worrying about it rather than acting on it, which I regret. So as I approach my 40th birthday, I know that it is highly likely this will be an on-going issue, as my consultant put it, “I’m on his Christmas card list’. So as I approach my 40th birthday, my birthday wishes include: •\tNurses who perform smears also have an awareness of vulvar disease and cancer, examine the vulvar area and ask basic screening questions about vulvar health. •\tGP’s are clear where gynaecological centres of excellence are and women are referred to these directly. •\tLet’s not be afraid to say the word vulva, either you have one, or someone you know does, so lets get over it. •\tWomen learn to know their normal – hold up the mirror, talk about it with people close to you, and the more people that do this the better. Normalise checking your vulva as you would check your breasts and don’t be afraid to talk about it/act upon something. I’ve posted about the issue on social media, knowing men would see it too, but remember men have wives, mothers, sisters and daughters too. Don’t leave them out or count it as a ‘female’ issue. It has taken me three years to ‘come out’ about my vulval cancer diagnosis. I was 29 when I was diagnosed with a rare form of vulval cancer, mucosal melanoma, and in one year I had five operations to try and remove the primary tumour with clear margins. I had just started working at my dream job, and nobody – least of all me – expected that I would need time off work due to a shock cancer diagnosis. And what could I tell all my new colleagues?
I told a few people that I had skin cancer – specifically, melanoma – and I got some sympathy, but not a lot of understanding. A couple of people told me that as a redhead, I should have expected a melanoma diagnosis (though mucosal melanoma is unrelated to sun exposure). At the end of business meetings, someone would inevitably take me to one side and show me one of their moles. Did I think it looked suspicious? Did it look like mine? None of these moles resembled what I’d had: a 4mm nodular growth that sat uncomfortably close to my clitoris. Outside work, I tried a different tack. I told friends that I had a ‘gynae’ cancer, and I left the rest to their imaginations. Some found a new way to blame me. Had I developed this disease because I had an STI? I heard more than a few jokes about my sex life. I tried to take the high road. Unfortunately, multiple wide local excisions could not ‘cure’ the disease. The post-surgery pathology results reported amelanotic (colourless, and invisible to the naked eye) melanoma that proved too challenging to detect and remove. I moved to a ‘watch and wait’ protocol, with regular gynaecology and dermatology visits, as well as routine body and brain scans managed by a melanoma oncologist. I enjoyed a few months of clear scans before the mucosal melanoma appeared in one of my lungs. The disease had progressed from stage II to stage IV. I had multiple tumours and this meant that I couldn’t have surgery to remove them. Instead, I started immunotherapy treatment (ipilimumab and nivolumab) – the standard treatment for metastatic melanoma. This time I only told a handful of people. I kept working during treatment and tried to keep my life as normal as possible. Immunotherapy didn’t give me any visible side effects so I was able to stay under the radar – but of course this meant that I didn’t get much support. Immunotherapy didn’t work. Melanoma doesn’t routinely respond to chemotherapy, so my next step was a targeted treatment on a clinical trial. There was no hope of curing the disease, but the trial drug was supposed to buy me six months of stability. I got married, went on a ridiculous number of holidays, and wrote my will. But the targeted treatment worked far better than anyone had anticipated – and as I write this, I’ve been taking the medication for 14 months and have had No Evidence of Disease (NED) for six months. For someone with incurable cancer, NED is as good as it gets. Nobody knows how long the melanoma will continue to respond to treatment. I’ve been wary about talking openly about my disease because of its intimate nature, and more recently I’ve struggled with the irrational fear that by sharing my lucky response to treatment I’ll somehow ‘jinx’ its future success. Starting my blog felt like a huge decision. I’m fortunate to have had access to phenomenal psychological support over the last three years, so I’ve never felt stuck for someone to talk to. As well as having a fantastic oncologist and trials nurse who always take the time to listen to my concerns, I have benefited from free therapy sessions at my local Maggie’s Centre. I can’t speak highly enough of therapy! It’s brilliant to have a non-judgemental, non-medical, sympathetic ear – and my therapist has helped me make sense of my diagnosis and my reactions to it. One of the topics I have yet to cover on my own blog is sex. Sex wasn’t really discussed during my gynae oncology consultations, although I had multiple wide local excisions rather than an immediate vulvectomy because my surgeon was working hard to maintain my sexual function. They hadn’t expected me to need so many repeat excisions, and my final operation resulted in a partial vulvectomy. Although my surgeon told me that my ‘vulval architecture’ had been preserved, i.e. all the nerve endings were still there, I no longer recognized my own body. I was struggling to keep up with all the physiological changes that had taken place in a relatively short space of time. Shortly after moving to ‘watch and wait’ (before I progressed to stage IV), I went on a retreat with the young adult cancer charity Shine Cancer Support. The long weekend (known as the ‘Great Escape’) involved a few discussions about sex after cancer, and I heard about psychosexual medicine for the first time. Why had nobody mentioned this to me before? It seemed as if I would almost certainly benefit from psychosexual therapy, but I was warned that there were relatively few practitioners out there – and if I wanted long-term support, I would probably have to pay. I wasn’t sure that I could afford to pay privately for this type of therapy – but I decided to explore my options and see if I had enough savings to fund a course of treatment. I didn’t know about the College of Sexual and Relationship Therapists at the time, but I’d seen a lot of adverts at bus stops in my local area that offered support to survivors of female genital mutilation (FGM). I emailed the FGM clinic to ask if they could recommend a therapist for me to contact. The FGM clinic sent my email straight to a psychosexual therapist in the NHS – as it turned out, the only person practising this specialty in my area – and two weeks later I started treatment via my local Sexual Health Service. I didn’t have to pay. I had multiple appointments over a period of two years, and as part of my therapy I was also referred to a trauma specialist who helped me to manage the PTSD symptoms I’d developed as a result of cancer treatment. My husband attended many sessions with me and we’ve been able to work on our relationship and explore the impact of my diagnosis together. Psychosexual therapy returned a sense of normalcy to our lives, and later gave me the confidence to start sharing more of my experiences with others. I found it very challenging to speak up about my diagnosis and the impact it has had on my mental health, but doing so has paid dividends. I was diagnosed with cervical cancer and then found out that it had spread to my vagina, bowel, bladder, 1 kidney, and the lymph nodes round my lower stomach in 2012.
I had radiotherapy treatment, which worked and I'm all clear. Both cancer and treatment have wrecked my body and I'm left with a few health problems, including lymphoedema. A few months after treatment I was having problems walking. It really hurt and i felt like my hips and thighs were congested and could only move in little steps. I just thought it was probably just because the cancer was located nearby inside me. I had been in contact with my Macmillan nurse, who are amazing and supported my every step from my diagnosis. And she suggested that I could go for complementary treatment in their centre at wythenshawe hospital. I was assessed there and it was arranged a physiotherapy session with a physio-lymphoedema specialist nurse. She immediately knew what it was and what to do. She pretty much gave me all the information and made sure I understood every little point. It was so comprehensive that I still use all that knowledge to this day. She advised my doctor to prescribe medical support tights which I have worn every day since. She also taught me manual lymphatic drainage and skincare exercise etc. I believe that if it wasn't for McMillan and their centre (which looks like a little log cabin) I would still be suffering with it now. They said it would never get better but I could stop it getting worse. I DID make it slightly better, though. My legs were regularly measured until they stayed settled. I feel pain every day but I'm still aware that it could be so much worse. I try my best to not break the skin on my legs and keep my weight down and to elevate my legs when they swell. It's a pain in the summer when they get worse in hot weather but every year it gets easier because of all the techniques I pick up. I make a spray with cold peppermint tea that is brilliant! The 9 months from August 2016 to March 2017 were a bit of a car crash for me.
In July 2016 I’d taken early retirement from my job as a Primary School Teacher. I wanted to have more time to enjoy my passions - climbing mountains, enjoying the great outdoors and exploring the world. Fast forward to the end of August when I was diagnosed with cervical cancer. Very tiny but very invasive. The word “disbelief” doesn’t really cover it. In fact, over 3 years later, I still expect a letter to drop through my door apologising for the mix-up with someone else. I didn’t feel ill, I felt fantastic. I was fit, healthy, happy. This was bonkers. Within days, I’d had a total hysterectomy, removing my ovaries, cervix, top of my vagina and nearby lymph nodes, just incase. I was offered radiotherapy and warned of the side effects. Ironically, lymphoedema was the side effect I most feared (since it might mean I couldn’t get out on the mountains), but since the side effect of NOT having treatment was a potential return of the cancer, I decided to go for it. 5 weeks of daily, external radiotherapy and 19 hours of internal radiation later, I was declared cancer-free. I was no more likely to get cancer than anyone else! Whooo hoooo! I literally skipped out of the oncology department that day. There may even be CCTV footage of it. My recovery went well. In no time at all I was back on the fells. My fitness returned pretty quickly and I looked back on it all as a minor blip. Life was good again. After a couple of months, I noticed my upper thigh was a bit swollen and sore. There was no bruising, so I presumed I had strained it climbing trees or something. It stayed swollen for a week or two, in fact, it seemed to spread. Funny. It was tender too. Strange. What could it be? Then came the light bulb moment. The one when “Strange…” turned to “Oh shit!” (Am I allowed to use profanity?) I popped along to my doctor’s with my self-diagnosis. She agreed. I’m afraid I was utterly dismayed. Not only could this take my mountains away from me, I was just getting over a divorce, following an abusive marriage. How would I ever find my forever man with such an incurable and disfiguring condition? Luckily, my doctor’s practice is outstanding. I was instantly referred to the Kendal Lymphology Centre, run by a nationally recognised practitioner. Within a short while, I was seen by a Lymphoedema Nurse who explained everything, showed me how to do the massage, taught me how to look after my skin, the importance of raising my leg as much as possible, etc and ordered stockings. Reading some of the stories of fellow sufferers, I realise that I am extremely lucky in getting such prompt and excellent care. I pulled my “big girl’s pants” right up and continued to climb mountains most weeks. I practised my self-care assiduously. It was hard and a huge mental adjustment but I had a strong word with myself. I was on top of this thing. It was a nuisance, nothing more. I could handle it. Positive and cheerful are my middle names. I did notice that my leg swelled quite a lot more after 5 to 7 hours walking up and down mountains and even more so, after then driving over an hour and a half back home again (I lived just outside the Lake District). It took a few days of doing not very much with my leg raised, to get the swelling back down to its usual size. And over the next year, it did gradually become bigger and bigger, in any case. The following year, in February 2018, I went to the Greek island of Chios. No, not the usual month for a Greek Holiday! I was going to help to set up and run a Children’s Centre for refugees. I had raised over £3,000 and was looking forward to trying to help some of the most deprived, disadvantaged and traumatised people in the world. It felt important that I should use my spare time and my skills to help. Unfortunately, my anticipated 3 months on Chios, turned into just a couple of weeks. My Lymphoedema went completely out of control. My leg was swelling up at a rate of knots. My skin couldn’t keep up with it and was really sore. I was scared. I came home, ashamed that after all that wonderful support from my friends, I wasn’t able to stay and do what I had promised to. Back home, it took weeks and weeks to get my leg under control again, albeit larger than it had previously been. But I gradually got there and set off climbing mountains most weeks again. Still suffering for a few days after each walk and subsequent drive home. By this time, I was getting used to the quips, stares and jokes as I went around in shorts and dresses wearing one thick stocking. In fact I bought some purple Lymphoedema stockings just for the hell of it! People weren’t being cruel. They just didn’t understand. I decided to become a one-woman-mission to explain to them! (Seriously, I am my own worst enemy sometimes!) I’m not pretending I didn’t hate it. I did. It was horrid. But I was determined to smile and be chirpy. Being miserable doth butter no parsnips. 12 months later, I noticed my other leg was feeling left out. It obviously wanted some of the attention. The Lymphoedema had spread to both legs. At this point, the profanities I’d like to use could offend the more sensitive reader, so I’ll leave you to imagine them. Let’s just say I was a bit miffed. And hey! Let’s look on the bright side! I now had matching legs! And today? I’m still climbing mountains. In fact, I have now moved house (from the village I’ve lived in and loved for 20 years and thought I’d stay in until I died) to be an hour closer to them - all because of the Lymphoedema. So that I can be home quickly to get my legs up. Where there’s a will… Does my condition affect my life now? Yes. Every single day. I have to plan my day to allow for time getting my legs raised enough. That means no long drives, putting my feet on the seats on public transport (and the dirty looks which ensue), 20 – 30 minutes of leg massage at the beginning and end of every day, wearing thick, black, hot stockings every day, all day. Struggling to find trousers which can get over my legs yet don’t fall down from my waist. I have given away all my shoes and started again, with what my mother would have called “sensible shoes”. I’m the one who sits to sing at choir, the one who has to get home after a trip to the theatre/cinema when my mates are going for a drink afterwards, because my legs are desperate to be raised. I can’t work with small children anymore – I was intending to do this one day a week after my retirement. I can’t volunteer at anything involving bending, sitting down or standing up. Which is everything really. I have to explain my condition when meeting people for potential relationships. (This on top of dealing with the various other “inconveniences” that Gynae Cancer treatment leaves me with – incontinence issues, problems affecting my sexual function…) I have to accept that I won’t be walking barefoot along a beach anymore. Or anywhere. On holiday, I swim in my stockings, because it is just so difficult to get them on again. I can’t sunbathe unless my legs are in the shade. Flights are possible but tricky. I need extra leg room and 2 or 3 days after the flight to rest with my legs raised, before I can start my holiday properly. Long haul flights are probably a no-no. Which is really sad because I was hoping to explore the world and volunteer abroad in my retirement. And don’t even get me started on the number of times I get cellulitis, leaving me really poorly for a few days and taking horse-pill-sized antibiotics for two weeks at a time! So, here we are. Do I wish I didn’t have Lymphoedema? Yep. Do I wish I hadn’t had all that radiation which caused it? No. Not at all. Lymphoedema is better than cancer, any day of the week. And although my condition is far, far less of a problem than many Lymphoedema sufferers have to contend with, I do work very hard every day to manage. I am absolutely definitely one of the lucky ones, but I do have to be vigilant to keep on top of it. And my mood. This thing will not beat me. I’m a glass half full kinda gal!
So when I had to have two lots of surgery to remove cancer from my vulva and lymph node extraction I put the lymphoedema leaflet in my ever growing medical file. I left hospital with a vulva the size of a small continent and one node site weeping! At this point no one mentioned that leaky wounds usually need antibiotics and to remain covered! So unsurprisingly I became very right side swollen as I had an infection. We all assumed that the swelling would go down as the antibiotics kicked in. However what then followed was a few months of a wound ejecting fluid in a very dramatic and terrifying way, swabs constantly taken to ascertain the correct antibiotic and pain in my pelvis, groin, buttock and pubis. Slowly the swelling subsided but my right side was , and to date still is painful and often swollen. It was at this point that lymphoedema was to be investigated. I had to be measure and probed for moisture levels to then be told yep I can confirm you have genital lymphoedema! Right I better dig the leaflet out and establish what this means. In layman’s terms lymphoedema is swelling caused by a build up of lymph fluid in the body but if the lymphatic system is damaged or inadequate it cannot handle the usual amount of lymph and fluid builds up in the tissues. So now I have to wear compression tights, slight issue I’ve been allergic to any materials other than cotton since I was a child! So I had to wait to have some special cotton ones made and when they arrive you get one pair, that you wear all day until bedtime. Pre operation I was a very flexible girl and proud that at fifty I could still do the splits and get myself in a crab position. Now I can’t even cross my legs! So getting compression tights on is like an Olympic event, coupled with the fact that half my vulva has been removed and I suffer from a chronic skin condition, vulva lichen Sclerosus. Which means I prefer to be commando and cool! I’m only recently diagnosed so I’ve just started having physio, I’m to be taught massage techniques and my lymphoedema nurse is exploring the use of low light therapy. I used to love driving but now it causes a dull ache and pain. Due to recovery time I am carrying more weight, which in itself does not help. To be honest it’s manageable but pretty exhausting and until now I’d been proud not to have had cellulite on my slim legs! I’m beginning to feel pretty gross about myself and everyday is a battle of what I can wear that’s comfortable and if I’m going to need pain killers to get through the days activities! Zoe Breen aka ‘flumpy foof’ My genitals are really weird now. You know those colourful stress ball things where you squeeze them and they pop out in different directions? That pretty much describes my lady bits since lymphoedema came a-calling. I had vulva cancer in 2018, they decided to remove the lymph nodes in my groin and within days lymphoedema had set up home in what was left of my vulva and isn't going anywhere soon! Since last years awareness day the dreaded lymphie has spread and is now from the bottom of my stomach to the ends of my toes, and EVERYTHING in between. This is me for life now and trust me, it sucks!
After taking myself to the Maggie's centre for counselling to get over my dread of being looked at and touched 'down there' I am finally getting treatment at our nearest centre. The nurse was lovely but why do they all insist on looking at me weird when I describe the pain and say “lymphoedema doesn't hurt”. Really? I can see from your chicken legs that you clearly aren't a sufferer. No litres of liquid trapped in your limbs? No opinion! With it being so widespread, and with my vulva skin being so roughed up from trying to escape the restraints of my extra wide gussets (knickers manufacturers please note; extra wide should cover area from leg pit to leg pit and not disappear inside the second it touches the Spanx!!) she decided in her wisdom to only give me something from the knee down. I also got a strange contraption to help me get them on. Point your toes like a ballerina, push through with gusto pull them up and voila! A very twisted American Tan coloured trainer sock without toes; no thank you. One trip to Amazon later and I'm the proud owner of 3 very sexy pairs of knee high socks is various colours and patterns. Pros; my legs feel a lot more supported when I'm walking Cons; my very expensive extra wide boots are now too bloody big for me and I walk with a wonk now and make a weird schloppy sound when I paid a fortune to look cool... Joking aside, lymphoedema is a complete piss take. •\tGet a garment to help one area and it makes another one worse. •\tDoctors and nurses talk bollocks; it is bloody painful. •\tWalking now feels like wading through treacle •\tHolidays during the summer are an absolute no go as with lymphoedema your legs and feet will swell to elephantine proportions and you will spend the entire time trying to keep your legs up, sweating through your garments and reminiscing about the days when you could actually get a tan below the waist There's times you get so frustrated that you just want to scream and cry and kick things but you can't get your bloody leg high enough ;0( So that's how it stands at the minute. I feel like one of those kids puzzles where you have to match the legs with the bodies but I got Popeye's top and Bluto's bottoms.. What was a bad day a year ago is now a good day. But what can you do? You open your eyes in the morning, breathe, get through the day as best you can then do it all again the next day, and the next, and the next.... Before anyone says it YES I know I'm lucky to be here! YES I cherish every day and look at life in a totally different way but it's just so f**king frustrating. When you're lying in a hospital bed with multiple tubes going into you and drains coming out of you, planning what you are going to do when you get out keeps you going. Then you get out and your own stupid body won't let you do all the things you dreamed of. Don't give up though, fight it! Fight for your right to live your life on your terms after all the shit you have gone through it's the least you deserve. I don't see myself as a loser, I see myself as a compromiser. I still want to go on holiday so I go at the beginning or end of the year and don't fly for more than an hour. My fact each one of my legs weighs about 10st makes it difficult for me to walk far so, at 53, I'm taking driving lessons. I may never cycle from Lands End to John o' Groats but I will go on a National Holidays mystery tour as my sense of adventure has reached a new high. Cancer may not be the death sentence it once was but with crap like lymphoedema as a lasting reminder it's still a life sentence. But, like any life sentence you can choose to spend your days wallowing in misery and self pity of give it the finger and make the most of every moment. It may not be how you dreamed life would be but hey shit happens :0) For two years, since the age of 5, my daughter suffered with:
- itchy pain in her genital area - sore & raw patches of genital skin - blood in stools - stomach cramps We spent many a night trying to comfort her, whilst she cried, wriggled and asked why it won't stop. Nothing would help, painkillers doesn't stop it, eventually she'd be so exhausted she'd fall asleep. It would last for days. I'd get calls from school to tell me there had been quite a lot of blood in the toilet & she was upset. Or that she was having bad tummy pains. We were treated (generally over the phone) for worms, thrush, constipation, given dry skin creams and were referred to the constipation clinic. 💙 This was all misdiagnosis. 💙 One January, after a particularly bad episode, I noticed she had raised, dark, blood like blisters on her genitals. It scared the hell out of me & I made another GP appointment. This wonderful GP took the time to look back over my daughters medical history and suggested that there's a possibility of Childhood Lichen Sclerosus. We were referred to a specialist. My daughter was 7 when we finally got the diagnosis, this was two years ago. The specialist said that GPs may only see one or two cases in 10 years in a child and it often gets misdiagnosed. My daughter and I took the GP a present and a card to thank her for taking the time to investigate this further and finally getting where we needed to be. The specialist said we just caught it in time before it has done too much, long term, damage. My daughter is now 9. Unfortunately there is no cure and it's a condition which just has to be managed with steroid creams & cuddles. There's a chance it may disappear at puberty. We hope. She gets flare ups, it's distressing, painkillers don't work, but we know that generally it will improve over a week. 💙 Be aware, look out for the signs, raise awareness 💙 I couldn’t tell you when this journey started for years I had this itch, was treated for thrush with cream and tablets that didn’t help.
Then I had my routine smear and they had to retest as there was a lot of bacteria there so they said I had bacteria vaginosis and put me on antibiotics, I thought great at least now they know what it is and they are treating it.Unfortunately not the itch went and by this stage it was doing my head in and thought I’m just going to have to live with it. Months and years went on and this itch got worse and then a open sore developed. By this time I was back for my next routine smear the nurse looked and said we must keep an eye on that broken skin you could have eczema and gave me a mild steroid cream which didn’t help much. Another few months passed and I decided back to the doc to see about this open sore. Well the doc didn’t even look and said could be due to starting menopause and gave me HRT suppositories, had my answer yes this will be the end of it. This was coming up to Christmas 2017 and had been going on for over 5 or 6 years. I used the suppositories all through Xmas and repeated my prescription in January but it wasn’t helping it was actually getting worse. It hurt to sit it hurt when I walked and the itch was so intense it kept me awake at night. February came and one day I was sitting in work nearly crying in pain got up rang my doctor to make an appointment and told my supervisor I was going. Saw the doc that afternoon she gave me an examination and said I needed to be referred straight away for a biopsy. Three weeks later I got my appointment to see a gynaecologist he examined me and said didn’t think it was too serious but would biopsy it anyway. Got my date for April for my biopsy after my procedure my gynaecologist came to see me and said didn’t think it was anything sinister and he would see me in a few weeks. Four weeks later I was sitting in my gynecologist office to get my results he said your biopsy came back you have vulval cancer. No words just tears , said we need to bring you in to have a radial vulvectomy this was double dutch to me. I cried all the way home in the car on my own. Got my phone call three weeks later to come in for my operation had a CT scan the day before my op on Tuesday 5th of June my 48th birthday. Had the op on Wednesday and gynaecologist said all went well they took some of my lymph nodes and he said they looked a bit nobly. Stayed a week in hospital and home to recover told me they would see me back in a month. A week later got a call could I come in to see my gynaecologist today. I knew this wasn’t going to be good news. He told me cancer had spread to my lymph nodes and I would need 25 sessions of radiation. Radiation was a nightmare first two weeks were ok but after that the burn started I could barely walk coming to the end of it. My dad brought me to all 25 session and said he could see me getting slower walking as the days went on. After it was over I had to go back daily to get the burns cleaned and dressed. Went back to work on the first of October thinking I could put it all behind me. But it’s always there in the back of your head I don’t think there is one morning I have woke up and not thought about what If it comes back. So June this year a year after my surgery I felt a small sore. It’s starting all over again went to check up and needed a biopsy went back for results and they told me there are precancerous cells . This is called VIN Vulva intraepithelial neoplasia. Also told me I hadLichen sclerosus which could of been the start of it all but was never diagnosed. So as I stand I’m waiting for my next operation and hoping and praying 🙏 I will be 60 years old next January . I was diagnosed with vulval cancer in May 2017 . I struggled to get diagnosed like so many others with this type of cancer . I underwent 9 months of brutal treatment as the cancer had spread to my lymph nodes in both groins. If I had been diagnosed earlier this probably would not have happened . I had chemotherapy , surgery to remove the tumour followed by plastic surgery and radiotherapy.
> > Chemotherapy … Now that was tough at the time and I had lots of side effects . The main long term effect for me is what they call Chemo Brain . It’s like an intermittent fog which makes you feel muddled at times .I also feel that my sense of balance was affected . I know I’m getting on in life and sometimes I put it down to an age thing but to be honest I was nowhere near as bad before the chemo . My skin has suffered since chemo also . I got white blotches around my eyes which never went away . My skin is a lot drier too. The veins in my arm that they used are lumpy and useless now and I have a large lump on the inside of my elbow which had to be investigated last year . They did an ultrasound and said it was nothing to worry about just a side effect of chemo . > > Surgery …My tumour was removed from around my clitoris . The plastic surgeon made a flap to close the wound . I am disfigured ,but to be honest I don’t think it looks too bad now . I lost my entire clitoris and surrounding area. The whole area has remained numb since the surgery . Obviously I have no sexual pleasure whatsoever now . No orgasms for me . I have been married for 36 years and and my husband and I always enjoyed love making . Now we have had to adjust to a new situation of no sex at all . What would be the point ? I feel really sorry for my husband . We have had to find new ways for physical pleasure . Never was I given counselling or was sex talked about with the medical profession . I was issued with hideous hard plastic vaginal dilators and that was it . I did try them and then bought rubber ones that were better but I hated them and it was sore, so I gave up . I was only using them in case I needed examined vaginally in the future . > Also when I pee now about 4 jets of urine squirts out all over the place and the whole area gets soaked . No matter how much I wipe myself after peeing when I walk away from the toilet a trickle of urine runs down my leg…….lovely NOT . > One of my groin scars from the lymph node removal (about 5 inches long) healed quite tightly and constantly pulls . It causes a pouch of lymphoedema to swell up over it like a lump . I gently massage it after washing but nothing really helps . > I don’t have pain from my surgery site as it is all numb . When I check things with a mirror I can’t find my urethra due to scarring and that worries me sometimes in case I need catheterised . > > Radiotherapy … Well this is the treatment that really threw me . I wasn’t informed of all the side effects from this ! I suffered severe burns on pubic area , vulva and inner thighs . I was in hospital on bed rest for 2 weeks . I didn’t know that you keep cooking after the radiotherapy stops . Like taking food out of a microwave !! Slowly the skin healed but has left unsightly red blotches and dark patches . It is also paper thin and prone to breaking down . It is very hard to ever wear underwear as everything I’ve tried can cause the skin to break down . I have spent a fortune on trying different pants and a huge amount of time scrolling the internet for suitable ones to no avail . > I had pretty bad bowel issues for the year following radiotherapy which I believe is common with pelvic radiotherapy . The worst time was the morning when I had urgency and sometimes didn’t make it to the toilet in time ….YUCK ! Mostly diarrhoea . Fortunately as time went on things have settled down . I take probiotics . > I have had 2 episodes of cellulitis following my treatment . The last one was scary and serious and I actually thought I may die( and so did my husband ) I was in hospital for 10 days in an isolation room as they found Strep B in my blood . All the intravenous antibiotics weren’t working but finally they hit on the right one ….phew ! I am now on life long Penicillin V which I take daily . Long term antibiotics can damage organs so I have to have 6 monthly blood checks ( not from my chemo arm ! ) > > Mental Effect …. All of the above is physical effects of my cancer treatment but by far the most challenging for me is the mental trauma that cancer diagnosis and treatment throws at you . Firstly you stagger out of the consulting room after initial diagnosis in a total daze . Totally unaware of what lies ahead of you . All through the treatment you are focused …. checking appointment dates and times , taking medication on time , reading up on stuff and working out what to ask at your next appointment . > When treatment finishes all that is gone and you have to adjust to the NEW YOU . Your family and friends say you look good and congratulate you on getting through cancer but really little do they know how much you have changed . I feel like a totally different person now and keep it all to myself as I don’t want to upset my family . I already feel so guilty for bringing this dark cloud to everyone . I wonder when it may return and when I will die . I went for counselling at the Maggie Centre as I was anxious and depressed suffering awful morbid thoughts . I am now more accepting of what’s gone on and try to stay positive . My therapy is enjoying nature , my dog walks and my beautiful grandchildren . This cancer journey has certainly been a mad rollercoaster that’s for sure . Sitting there on the hard plastic chair, my hands clasped tightly in my lap, I asked the consultant to repeat herself.
‘The doctor you saw on your last visit was correct. You have Lichen Sclerosus.’ Nodding, I listened as she outlined the disease. Of course, after my last visit here to the GUM Clinic when the doctor had hinted that the discolouration ‘down there’ may be Lichen Sclerosus, I had googled it. Everyone does, don’t they? Now, sat in the small, stark room I tried to focus on what she was saying. Her words muddled with the research I had gleaned on the internet. I needed to listen, I needed to get the real facts. After all, everyone knows that Google churns out the worst case scenario. Everyone knows that you can Google a papercut only to be told you have a fifty percent chance of your arm needing to be amputated. It’s a well-known fact that that’s how the websites get their hits, by sensationalising the normal. This Lichen Sclerosus thing can’t be as bad as all that. Some of the things I’d been reading… Shaking my head, I tried to shut the thoughts away. ‘If you look here.’ Leaning forward, my left foot tapping on the floor, I peered at the photograph on the camera. Not in a million years did I ever think I’d be asked to gaze at a photo of my own vulva. ‘We’ll keep this photo as a base and then when you come back we’ll have something to compare any changes to. Of course, you can ask your family doctor to refer you to the hospital, if you’d rather?’ Shaking my head, I swallowed the bile stinging the back of my throat. How could I go to my family doctor and show her this? Nodding, the consultant shifted in her seat and picked up a pen, using it to point to the various parts of my photographed vulva. ‘Here, you can see the tell-tale grey-white patches on your skin. You can also see here, and here, that your labia minora has fused with your labia majora.’ Biting the torn cuticle of my thumb, I blinked. ‘You mean I’ve lost my inner lips? They’ve just gone?’ ‘I’m afraid so. Your Lichen Sclerosus has resulted in them fusing.’ My Lichen Sclerosus? Mine? I don’t want it. I don’t want the stupid Lichen thing. And how could my inner lips have disappeared? How could I not have noticed? I mean, I’d noticed something was up, something had changed, but not in a million years did I think this had happened. Or that it was even possible to literally lose part of your body. I’d thought I was going mad or something, I’d thought I’d remembered it wrong. Why hadn’t I taken more notice of my own body? Why hadn’t I come to the clinic when the nurse had first said something looked different? I wrapped a strand of loose hair around my finger. I’d had my smear, what, four months ago? It had been then that the nurse had said there were a couple of patches of grey down there. She’d told me to go and see my doctor. But, of course, me being me, and getting embarrassed by stuff like that, I’d gone to see a different doctor, one I wouldn’t have to see again and again for various other things. But this other doctor had said it was probably fine, she’d said it was probably just me, not anything to worry about. She’d advised me to go and get it checked by the nurse who specialised in family planning at the surgery. And I had. And she’d said the same, that it was probably just me, that the skin had probably just changed colour slightly, more than likely due to my age. I should have come straight to the GUM clinic. I shouldn’t have left it so long. Why had I? I shook my head, I’d had three people tell me it was probably nothing. That’s why I hadn’t. I’d trusted them. I’d taken their word as truth. Taking a deep breath in, I bit my bottom lip. It wasn’t their faults, it was mine. It was only me who hadn’t taken my health seriously enough to get another opinion. Plus, the symptoms wouldn’t have been as severe back then. That was probably why they hadn’t been able to diagnose it. Still, though, if it had been diagnosed back then, I might not have lost half my vulva. ‘Will it come back? Will it unfuse?’ Leaning forward, the consultant kindly patted my hand. ‘No, I’m afraid the changes are irreversible, but what you do now may prevent any further changes.’ Further changes? What else could happen? ‘But I’m only 39, isn’t it something that’s supposed to affect postmenopausal women?’ ‘Not always, no.’ ‘I haven’t had any symptoms, though. I haven’t had any itching or any pain, only a bruised feeling when I spend a long time on my feet.’ Can it really be a silent disease? Can it really change the structure of my bits without any warning signs? ‘You’re right, its more common to have itching, soreness and even pain with Lichen Sclerosus, but it’s not unheard of not to.’ Leaning back in my chair, I closed my eyes. Why me? Why did I have this? It didn’t make any sense. None of it did. ***** Fast forward six weeks and I’m sat holding my mobile to my ear. ‘I’m sorry, no one is available to take your call. Please try again later.’ Folding the hospital referral letter, I slip it into the back pocket of my jeans. It’s fine. I’ll try again later. And again. And again, until I get to speak to a human and make an appointment. You see, I’m ready to take control. I’ve done the crying, the grieving of taking a ‘normal’ vulva for granted. I’m ready to block out the feelings of despair and sorrow that keep trying to rear their ugly heads. It’s not easy. Some days all I want to do is crumble, hide away from the frightening realities of this disease and pretend it’s not happening. And some days I do. But not every day. I’m not going to let this thing, and the fear it brings, control me or my life anymore. And I’ve already begun, I’ve begun taking control. I plucked up the courage and went to see my regular doctor. I asked for a referral. I’ll get the help and advice I need, as soon as I can make an appointment anyway. Until then, I’ll continue to follow the advice I’ve gleaned from other sufferers. I’ve upped the frequency I use my steroid cream and I now know to apply my moisturising cream religiously, not just when I remember or when it’s convenient. Yes, I’m not the same as I used to be down there and I never will be. Heck, it’ll probably change again, and again, and again. But am I going to let this disease and the damage it’s doing define me? Hell no. There’s more to me than that. I’m still who I was before this nightmare began. I’m still me and nothing can take that away. Thanks to the Lichen Sclerosus UK Support Group for Women on Facebook, I now know the recommended protocol is to use the steroid cream twice a day to begin with, not the once a week I was originally told. Now, I have hope. I have a way to try to regain control of my body and thanks to the group, I have the support I need whilst I do so. Age: 56
Living in Taiwan 1978 Reynaud’s syndrome 1992 Hashimoto’s thyroidism and Coeliac disease 2014 Bilateral mastectomy (Invasive Lobular and Invasive Ductal carcinomas) 2016 Oophorectomy 2019 LS Mid February, 2019 I felt a soreness and itch around my clitoris and labia. A discomfort that, after a couple of nights, became a burn in the whole vulval area, making sleep elusive. After a week I suspected that a recent change in washing powder was the issue and switched to hypoallergenic, fragrance-free products. Late February The burn, itch and pain was becoming worse. In fact, I was feeling the symptoms all the time. To make matters worse, every time I had a bowel movement, the pain was intense (like passing glass) and I would bleed badly. I was meticulous about keeping clean (having a wonderful Japanese toilet that sprinkles and spurts water wherever and at whatever temperature and force desired) but nothing seemed to work. I used Sudocream hoping it would relieve the anal pain but each toilet visit had the same, bloody outcome. Early March Visits to two colorectal specialists for the pain and bleeding provided no answers (even after a colonoscopy) and I was sent away with haemorrhoid cream and the suggestion I look into IBS. I’ve been coeliac for 27 years, lactose intolerant for 9 years and am extremely careful about my diet. However, I did research and started a low FODMAP diet. Surprisingly, this did help a little. I bloated less, was able to do a number two more frequently (now every day or two) and, being softer, I did not feel cut as badly. Mid-March My vulva, labia and clitoris were more painful than ever and felt bumpy. Examining with a mirror,I could see that my labia were shiny white, with hard patches, and so, the very next day, I visited a familiar gynaecologist. “Old woman’s issues” I was told - he recommended using Vaseline and said goodbye. Late March I used Vaseline for the week I waited to see my specialist gynaecologist (he had performed my keyhole surgery) and, having used Google to research my symptoms, I was convinced that my issue was more than becoming “old”. The specialist looked, booked a biopsy for the following week and gave me Bestasol cream and Hyalofemme lubricant. The former cream did help (it was a mentholated Clobetasol), whilst the latter made me itch more and so I abandoned it after a couple of tries. Early April Results were in and I was told... “Leukoplakia. Hormone treatment can help but not in your case (my cancers are hormone receptor positive). Keep using the cream.” ... and that was it. Happily, the cream began to lessen the patches and the whiteness on my labia. (While he called my issue “leukoplakia”, my medical records show the biopsy result as “Consistent with LS”) Early April One of only 2 doctors in Taipei whose medical specialism details mentioned LS, was seen. She, whilst remarking that I was in a severe flare, recommended a different hyaluronic acid product to moisturise and talked about PRP therapy and laser therapy. The gel was expensive (£125 for 4 individual use tubes) but the therapy was prohibitive at £3,000 per treatment and 2-3 treatments needed per year! I tried the gel but did not see any noticeable improvement. I returned to using Bestasol. Unfortunately this is when the fusing became very noticeable. End April Surgery was discussed with the other specialist who had LS experience, and she scheduled a small procedure to release my half-fused clitoral hood. However, I ended up with the labia being separated and internal incisions at 12 o’clock and 6 o’clock to counteract the shrinking of my vaginal opening. 5 weeks later the stitches were removed. July I obtained a tube of Dermovate cream and tried it, hoping it would reduce the redness that had replaced the whiteness and patches. Unfortunately it made the redness worse and started me itching again. At this time though I discovered, for me, that ‘washing’ with coconut oil seemed effective in managing the itch/burn. I also discovered local water wet wipes that I used after every toilet visit, with comfortable results. I felt that I was in remission. October The stress of how I felt, the realisation that I was losing all that was anatomically female about my body, really hit me hard: No boobs and disappearing lady parts was unbearable. Consequently, I suffered from mood swings, with frequent outbursts of anger and/or tears. Early November I started counselling to help me deal with the emotional aspect of the issue. I also joined your Facebook group and reading about others in similar (awful) positions helped more than I can express. 31st December 2019 My 56th birthday! Life is not easy: 11 months ago LS did not exist for me. Now, in addition to always needing to be conscious about where and what I eat/drink, I also need to be prepared for using toilets outside of my home and for activities that may trigger flares (swimming/hot springs/long journeys, etc). Fortunately, I have the most amazingly supportive and loving partner who continues to make me feel beautiful and helps me to be brave and organised. I’m also very grateful that your group has given me more clarity than any doctor and more tips on what to try. The goalposts constantly move but you help me to respond. In spite of using Epsom Salt or Dead Sea Salt baths to try separating small sections of re-fused labia (occasionally the skin did split) the fusing continues. I have an appointment scheduled with a doctor famous in Taiwan for his holistic approach to palliative care. Recognising that none of my conditions are life threatening, he has, nevertheless, expressed interest in exploring using similar treatments and strategies for me. This fight will go on, and my life will be lived to the full I was diagnosed a couple of years ago, albeit I allegedly had it for years before but was treated for bad thrush etc. I was prescribed Canesten cream, which I used virtually all the time.
I am nearly 70 now and have not had sex with my husband for many years. I used to joke with my friends that if I didn’t have to wee, it would close up. Anyway, one day whilst wiping myself I couldn’t feel anything, it felt “closed”. I lay on the bed and felt the “closure “ I tried to pull it apart but the pain was indescribable and blood everywhere. I managed to get an appointment with a locum who immediately diagnosed me with LS. Because of the length of time without diagnosis, she fast tracked me to oncology gynecologist. He was certain there was no cancer and requested my GP to refer me to Ls specialist. Trying to see a consultant was a nightmare and i was pushed from pillar to post. I eventually paid privately to be seen by the consult indicated by the gynacologist. She runs a joint Dermatology/Gynecology clinic weekly at my local hospital but “The Board” refused me access due to funding. After a year of fighting I was eventually referred through the Gynecology department. Unfortunately the specialist surgeon left in September and i have to wait until January to see another doctor. I don’t think she is an LS specialist, if not I shall just have to pay privately again. Being a pensioner, this goes against the grain. Through the joint clinic, i was prescribed high doses of amitriptyline and then prednisolone. Unfortunately I couldn’t tolerate these high doses so came off amitriptyline and weaned myself down to 5mg of prednisolone. I was also prescribed Nerisone ointment to use daily. Unfortunately the manufacturers are unable to meet demand. I have just enough left to see me through to my January appointment! None of the GPs in my surgery had heard of LS and none of the nurses were aware of it either. None of my friends had heard of it either. What a sorry state of affairs. At around 13 years of age I started bleeding from my back passage. Not a lot, just a sting and then blood on the toilet paper, but I knew this wasn’t normal and I was old enough to know that it could be something serious like cancer. I hid it for a while, as you do when you’re young and scared, but eventually told someone and a few months later I ended up at my local doctor’s surgery. They examined me, and told my mum there seemed to be nothing really wrong, and I should simply increase the fibre in my diet and the bleeding - and itching - was put down to haemorrhoids.
If that doctor had known more, my Lichen Sclerosis might have been diagnosed then. But they didn’t, and nor did I. The thing is, when you itch a lot of the time, and it starts about the time that your body is changing in all sorts of other ways, you just assume that’s a normal feature of puberty, right? If it got really bad, I assumed it was thrush and treated it accordingly. The flare up would ease and I’d go back to long-term low-level itching. I didn’t talk about, so the fact that no-one else talked about it seemed perfectly normal. And so it went, for about 15 years, until one day I woke up and down below was smelly, itchy and sore and something was quite clearly Not Right. I took myself off to the emergency sexual health clinic, and waited with many others, who were worried about pregnancies, STIs and who knows what else. I was eventually seen by a wonderful man whose name I have since forgotten, which is something I regret very much. He told me there were three different problems going on at once: bacterial vaginosis, thrush and something called Lichen Sclerosis. He explained that it was rare (something I’ve come to doubt), may eventually lead to cancer (that childhood fear again) but easily treatable. He furnished me with a suite of medicines to treat all three conditions and in doing so, changed my life. In the following weeks, the steroid cream he gave me began to work, and for the first time since I was a child I realised that people didn’t just itch all the time. It was a revelation. I returned to that doctor for a routine follow up and he told me more about LS. He also explained that the area around my labia, including my clitoris, had fused in various places. I wasn’t a terrible case, but the untreated years had taken their toll. He told me at that appointment that he had been offered a new job in London, and I never saw him again. In the intervening years (I am now 40) I learned that I couldn’t do without the steroid ointment. No matter how rigidly I followed the recommended regimen, anything more than a week off the steroid - even after intensive treatment for months - was enough for the itch to return. I learned that some emollient creams and other meds have ingredients that cause a flare-up for me, even though they suit other LS sufferers just fine. I learned that many health professionals don’t recognise LS, and that people who have been treating ‘chronic thrush’ for years probably don’t have thrush and maybe never have. I discovered that my best friend developed the disease after giving birth, and that it is likely much more common that the literature suggests; it’s just not so common for people to be diagnosed. If I’d spoken about my issues more openly, perhaps she’d have been diagnosed sooner. At the moment, I have my specialists’ blessing to continue to treat my LS as I see fit - I am now the expert on my own condition, which feels fair after living with it for longer than most professionals have been qualified. It remains under control as long as I treat it regularly with steroid ointment, moisturise properly and don’t allow fragranced products to come in contact with my nether regions. I’ve started using a menstrual cup, which has definitely helped - the silicone is skin-friendly, and the manipulation it requires to insert and remove means I’ve both stretched out some of the fused areas and felt more confident that I will stretch without tearing now. I contracted genital herpes via my husband’s cold sore (yay!) and learned that we LS sufferers are more prone to it than most. This time last year I finally did get that cancer diagnosis I feared as a child, but it was cervical cancer, and not related to my LS. It was caught during a routine smear test and I never knew I had it - it was excised in the biopsy to find out what the abnormal cells were, and I treasure the letter telling me there is no residual sign of the cancer. I spent so long dreading my smears, especially because the fusing left me with tightness and a fear of tearing, but I’m glad I kept up with the appointments. The future seems bright to me. I am told that the concern about the steroid ointment thinning our skin is based more on statistical possibility rather being a definite outcome. It may happen, but the warning on the label is there to protect the manufacturers rather than as a ‘this will definitely happen’ prediction. I am well-looked after by my healthcare providers, have stopped the fusing, and begun to reverse its effects by stretching my skin, and stay diligent about fragranced products. I remain very grateful to that unknown doctor who diagnosed me 12 years ago. Unfortunately, vulval cancer tends to be like a really bad film franchise, it just gets shittier and keeps coming back.
(I've actually lost count of how many surgeries I've had in 9 years since Diagnosis Day) . Some big blockbusters in there: Vulvectomy, Excision of the Sentinel Lymph Nodes, Marsupialisation of Bartholins glands. Others the less impressive: Laser (feat:Burn baby Burn) WLE, WLE the Revenge and WLE Reloaded (wide local excision) Topical Chemo starring Chemical Burns , Punch biopsy 1, 2, 3, 4.... So, The Return of the VIN (vulval intra epithelial neoplasia = dodgy precancerous cells/cancer in situ) is pretty much anticipated every 3, 6, or 12 monthly check up. Post surgery complications are for life, not just Christmas, and include the Academy Award winning Pain, Lymphoedema and Disfigurement; Depression, Anxiety and Sexual Problems plus the likely winner: 'No sex please we're vulval cancer survivors'. This means that life post vulval cancer can be more of a mystery/horror story than a perfect happy ending. #vulvacancerawareness #fuckcancer Back in 1996 I had Hysterectomy operation I was close to forty years of age. I had uterus removed and a small cyst removed from my ovaries which they didn’t remove. I had a prolapsed womb, my bladder was pressing on it the muscle that held it in place needed repairing which they did .
Every thing was fine, I was given Hrt patches. I had started getting UTI's and Thrush, Breast cysts which was drained at my local hospital on and off through out the years, used over the counter medication drinks unless I couldn’t clear it up myself. I would go to my Dr, I was having. U TI's as long back as I can remember after child birth, 2 Episiotomy and one tear. I was taken off Hrt when we discovered it would be safer for me not to have it seeing as I kept having cysts in my breast. After I had turned 55 ish I didn’t get any more cyst and everything was okay, still had the odd one or two UTI's. Until one day my dr said I need the help of vagifem pessary, what a big relief 3 years I have been using them so far . I had camera test done CT scan to see if my ovaries were enlarged , gladly they had shrivelled up which is a good thing, had polyps removed from my bowels which were tested and were fine no problems there. Last year I had to see my Dr about them because I had three, what I thought were water infections close together. This year Dr said that there wasn’t any infection and it could be very likely VA and dr at hospital gave me antibiotics to treat it. I was sent for a fast track appointment by my dr at new cross Hospital to examine my vagina and to look for anything nasty. She was concerned about the redness and lesionS. This was back in beginning of September. I was checked out by hospital gynea who told me it wasn’t cancer, could be lichen Planus, to carry on with vagifem and clob and said I would get my next appointment through the post in 6 weeks, it will be 9 weeks this Monday and haven’t heard anything from Hospital. Good job I found Jane Lewis on Face Book and all the tips I have picked up off there, I have gladly, everything under control with me and my vagi ointments, moisturisers and oils plus vagifem twice a week. I’m good not perfect but much more bearable. Thank you for listening From June Guest, Age 64. I first became aware I had this terrible disease when for no apparent reason I couldn’t stop itching and burning out of the blue one week almost exactly a year ago! I remember the time because we were due to go on a celebratory cruise for joint 50th and 60th birthdays for my husband and I and also as a delayed honeymoon.
In recent years intercourse had been problematic for us for quite a while, my husband has prostrate cancer and after having biopsies, it had left him with erectile dysfunction. I would also need an antibiotics every time to stop the reoccurring urine infections that I would get every time we made love. I also have Fibromyalgia and am registered disabled so am used to unusual pains etc. However this burning and itching was something else, I also noticed one side of my labia seemed longer and thicker than the other. I booked in to the GP, she didn’t say anything but agreed to send me to see a consultant gynaecologist . As I have a private health care scheme and was going away in 7 days I told her I would see someone privately first of all. My first appointment was at a BMI Hospital. I saw my consultant, who barely spoke to me. She asked me to pop up onto the couch, had a quick look. As I was getting dressed she told me I had Lichen Sclerosis , that I needed to apply this steroid she was going to give me very liberally, all over 3x a day that I should get through 3 tubes in about 1 month when she would review me for a biopsy to make sure there wasn’t any cancer, and off I go! My head was swimming!! I had just been given a diagnosis for what? What is it? What happens now? Will it go away? Why do I need a biopsy? What was this medication? I came home and cried. Then I looked up the words Lichen Sclerosis and found the name Jane Lewis, I messaged Jane on messenger and explained what had happened, she gave me the details of the the Lichen Sclerosis UK support group on Facebook. This turned out to be my lifesaver. Thank goodness I listened to my wonderful friends/family on there who said” how much dermavate”!!!!!! You will be red raw!!!!! So I only put on the normal twice daily etc.and was guided by my wonderful experienced ladies and pharmacist. After returning from our cruise I decided to see another consultant as my LS was still out of control and my Vulva was looking very strange. I researched and found a lovely consultant locally. When I saw her she was indeed excellent and it was such a different experience. She took the time to explain what LS is, where exactly I have it, she then gave me a whole leaflet on the best ways to look after it how to get into remission. Then she said that she didn’t think I needed to go through a biopsy as it was too stressful and that someone like her was experienced enough to see and judge it. I explained to my consultant that I couldn’t afford to see her any more privately and she said that’s not a problem as she would ensure I could see her on her NHS patients list. A fabulous, kind doctor who even took the time several time’s to follow up with emails sent home. I left with more knowledge on how to use the dermovate and on a strict regime of using it with moisturisers etc. Finally my NHS appointment came through, at this point my LS was again out of control due to going through an incredibly stressful time. I went along to it, only to find I’m under a different doctor yet again. He takes one look, says “ hmm not sure what that is, but don’t think it’s LS ( even though I showed him the letters from both other consultants) then he calls in a more senior doctor who then agrees with him! They then decide I need a vulvoscopy and to be seen by a Vulva specialist. But this again can take time and if I could go privately I should. Again I’m bleeding with an incredibly sore Vulva my shape is changing rapidly, so I ask my private Gynaecologist who she would recommend. Then I go and see this fantastic lady a Vulva specialist. . Again this lady takes one look, says it’s LS with moderate -severe vaginal atrophy, this is actually the first time anyone had said these word. I knew this, but no one had confirmed it!. I felt sick, now it had been confirmed, my worst nightmare. She says she doesn’t need to do a Vulvoscopy straight away but can do it later on, as I’m booked in on the NHS I may as well have it done there anyway. . I get the pricing for it privately anyway just in case, and I’m covered. But she also says I can see her in the NHS. She gives me loads of advice, everything from diet to what to wear. She has now also included 2x a week vagifem into my meds to help with the VA and said to use coconut oil in the morning and dermovate in the evenings only now. My appointment for the NHS arrives, for my vulvoscopy and to see the consultant. I’m expecting to see my consultant but alas it’s to see another doctor but someone who I’ve heard is excellent. As before however they need to change the appointment. When they reschedule it, I make sure there are the two appointments together, vulvoscopy and consultation. I go along and wait for over 90 minutes for a 09.10 appointment. I see this lady who asked a few questions, re what meds am I on how long have I had symptoms, I try to bring up my vaginal atrophy and my menopause symptoms to see if she can suggest extra Vagifem or HRT as has been pointed out in the groups. Her reply is simply “ I’m only here for your Lichen Sclerosis, you can ask your GP about those things”!! I honestly couldn’t believe this. She then asked if she could “take a look” and that she had a student with her so would I mind? At that point I was so pissed off if the entire Welsh Guards came in I just didn’t care. She had a quick look, did an internal where she said my vagina was extremely tight as well as the pudental nerve suffering from being over stretched . She followed that with a “you can get yourself dressed now and we can talk over by my desk”. She told me that she wasn’t entirely sure if I had lichen Sclerosis, but that I was extremely tight and that my pudendal nerve was overstretched! She also said if I wanted she could organise some physio for my tightness, but it was up to me at this moment in time? Then she showed me how to sit and loosen my pelvic floor muscles which are way way too tight! “ By now I am so fuming I can barely speak, not only has she refused to answer my questions on my vaginal atrophy but she also hasn’t done the vulvoscopy which I was booked in for… plus she is guessing about my diagnosis! I couldn’t get out of there quickly enough! I mumbled something about not taking up the physio yet, then she simply gave me a piece of lined paper with dates on which she asked me to record what I used each day for the next six months, before handing me a sheet to book again in 6 months time. I was in and out in about 10 minutes. After this awful appointment I telephoned the secretary to ask to be moved from her clinic to one of the others clinics. Her secretary actually had the Gaul to argue with me! When she said why, I replied that I was supposed to have had a vulvoscopy and it wasn’t done. The secretary answered “ do you even know what that is? She had a look at you didn’t she”? To which I replied” A vulvoscopy is where they place an avid over the Vulva and look through a special microscope! She went very quiet, and simply agreed to remove me from her list and hand me over to the others. Why is everything such a battle for us. I’m now waiting for my new appointment to come through and with any luck it will be with my lovely Vulva specialist, but then again in my experience. Who knows. Meanwhile I’ve been back to my wonderful GP who has put me on HRT so for now I’m just hanging in there. I had grown up with endometriosis and the lack of GP knowledge over “just sore periods” and being told to have babies as that would fix it! Roll on to a ruptured ectopic and 9 miscarriages, none explained but possibly down to my endo. At 44 I decided to get sterilised as I could not go through any more emotional or physical losses. GP said no but referred me to gynae who agreed. I was told that my remaining ovary (remember the ruptured ectopic) was cystic so they removed it. Nothing else was explained. About two years later I felt awful, it was like I had 3rd degree burns in my groin, all around my vulva and going all the way back to my bottom and beyond. GP took swabs and gave me steroid cream. It didn’t work, I was in severe pain and my marriage and work were suffering. Eventually I was referred to the Colorectal unit! Why I asked? Well it could be piles!! After very invasive and painful examinations such as colonoscopies etc the consultant said there was nothing he could do,oh by the way are you in the menopause yet? You could have slapped me! Menopause? Surely not! I feel stupid because although I know a lot about my reproductive system, I would wouldn’t I, it had never occurred to me that the loss of that final ovary would have sent me down that rabbithole to Menopause land. I started investigating and went back to GP who insisted on blood tests! Pointless if I have no ovaries but what the hell, had the tests, yes you are perimenopausal. No advice, nothing. I was so low, no sex, felt like I had the flu, my genitals were on fire and obviously this was sending anxiety sky high! It took me two years to get HRT, sequential to begin with which flared my endo so I demanded combined as I still have this useless uterus, see I was now educated in HRT? My GP and nurse weren’t, this HRT was going to shorten my life according to them! Poppycock! The burn and cuts on my vulva were still making my life a misery, to the point of suicidal thoughts. Pain on sitting, pain on standing, pain on lying down. An excruciating need to scratch so I ended up wearing mittens to bed, like a bloody baby! Eventually I self-referred to the Sexual Health Clinic. In the Highlands we no longer have a Menopause Clinic! So off I went, in disguise, surely only STI patients need sexual health? This consultant actually examined me! She was shocked at how severe this thing called Atrophy was! Atrophy I asked? Well now with a brain full of even more knowledge and a nice hospital prescription of Vagifem pessaries, antibiotics, steroid cream and lidocaine off I go. Things started to improve, it was a bloody miracle finally! Then it came back. Multiple appointments later I’m told vulvodynia. Nope I know it’s not, check me for LS please. Biopsies and swabs show no LS thankfully but what is happening? Just use the numbing Lidocaine to re=educate your nerves!!! I’ve been going round in circles! GP is now fighting me over HRT, Vagifem and Estriol cream, the things that make my life liveable. Through groups of other women I have found out that Lido thins the skin even more! I can’t get transdermal gel in my area so I’m taking oral combined HRT, no surprise the GP is trying to scare the life out of me. It is a daily struggle to be a wife, do a job and not just give up. The physical pain, the mental torture and the constant thoughts of “is this going to be forever?” It hurts to pee, itkills to poo and my inner vixen has run away. I jump in meetings often, like I’m stabbed, I make excuses, die a little inside and just get on with it, this miserable existence focussed on my genitals that no longer even allow me to be myself. Vulval cancer. Life after.
As a married woman, and mother of 3 amazing children (aren’t they all). I headed into my 39th year, feeling invincible, having a better understanding of my life, myself and stuff in general. Jan 2017 rocked my world! And not in the best of ways. I’ve always been sick and almost held hands with death at some stage, but hell !! This new surprise , I thought, beyond me. My consultant, after much pushing , utter the words no one wants to hear, the word that means the end of all ends. I had cancer and not any “normal, well supported, talked about cancer. Nope I could have won the lotto, but I got a cancer that in some peoples minds is an easy cancer, wtf?!?!? Oh yeah, for me it was easy, compared to most of the amazing ladies I have since “met". We are few, but we matter. I had the terror of the actual diagnosis. I reasoned my eldest was old enough to remember and live without me, she was 18. I was distraught over my younger 2 (10 & 12). I went in for my surgery 5am on the day, no idea what was going to be done until I was on the table and asked him to draw me a diagram. Holy hell, half of my “lady bits" were being torn (dramatic, but that’s what it felt like) from me. My surgeon could not guarantee I could still have a sexual relationship with my husband post OP, but worse he could not guarantee he could stick to the plan. Depending what he found would depend on how much I would lose. Post op day one, I was told all went very well, no extra surgery was required, BUT .. he had to take more than he thought and stitching was tight, so the question of sex, which was the last thing on my mind, was an unknown. My husband joked that he hoped his private health insurance would cover any nessecary repairs. It was a long, painful recovery thankfully with no other treatment. And I have been so lucky and glad of the support around me. My kids, still drive me nuts, but I love them. My husband also drives me nuts but had been my everything! Patient, kind, supportive and just present. And yes there is life, love and intimacy after vulvar cancer. Ailis |
AuthorWrite something about yourself. No need to be fancy, just an overview. Archives
August 2023
Categories |








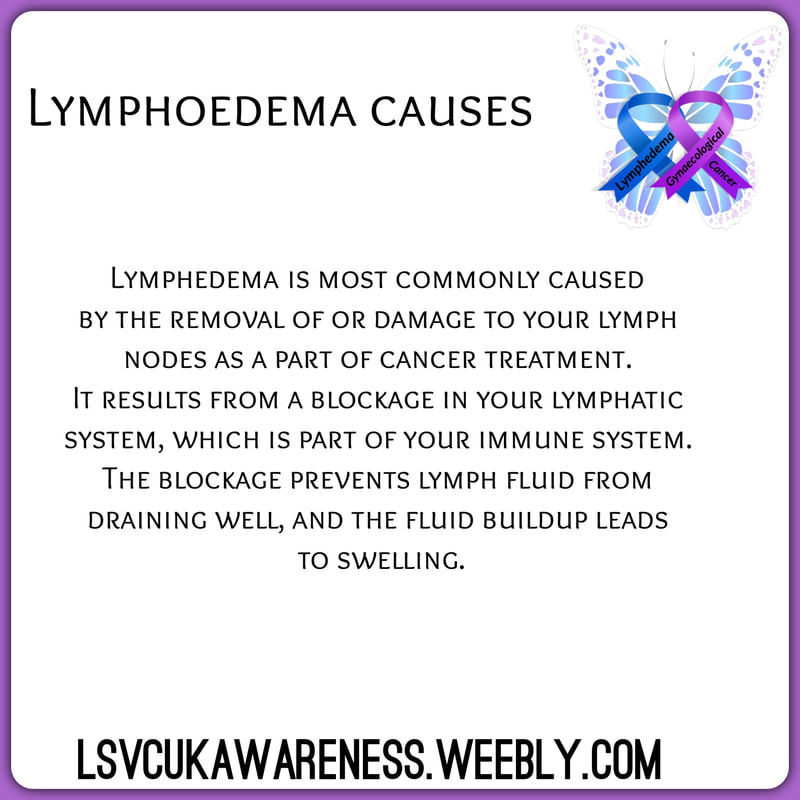
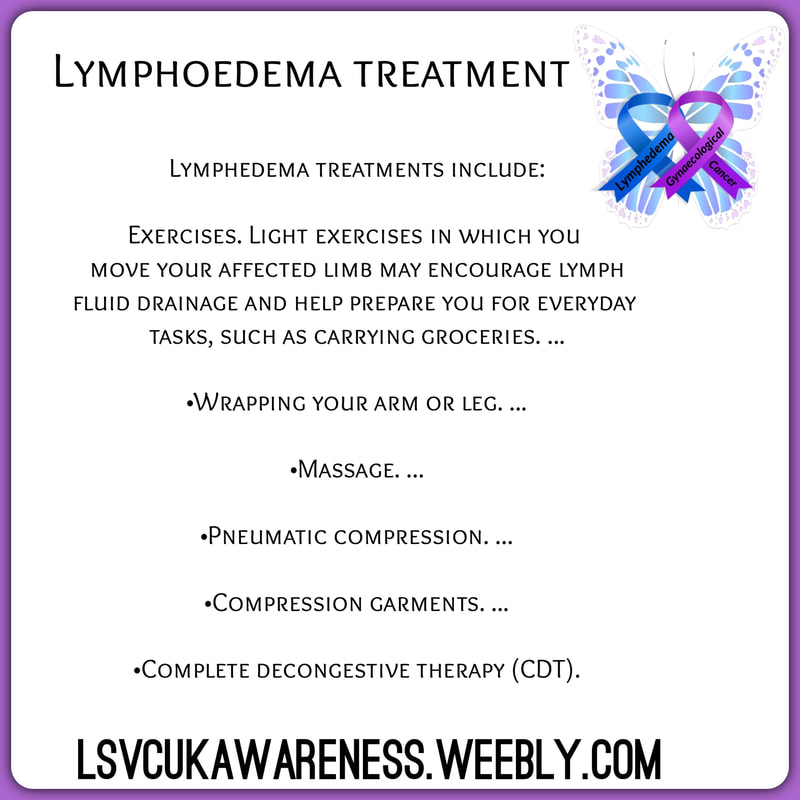
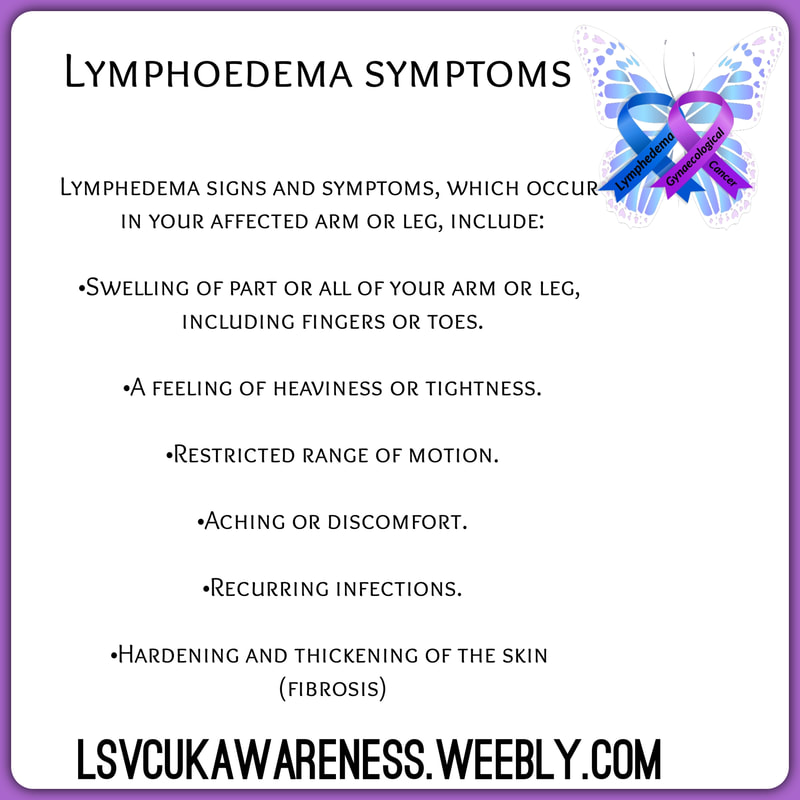
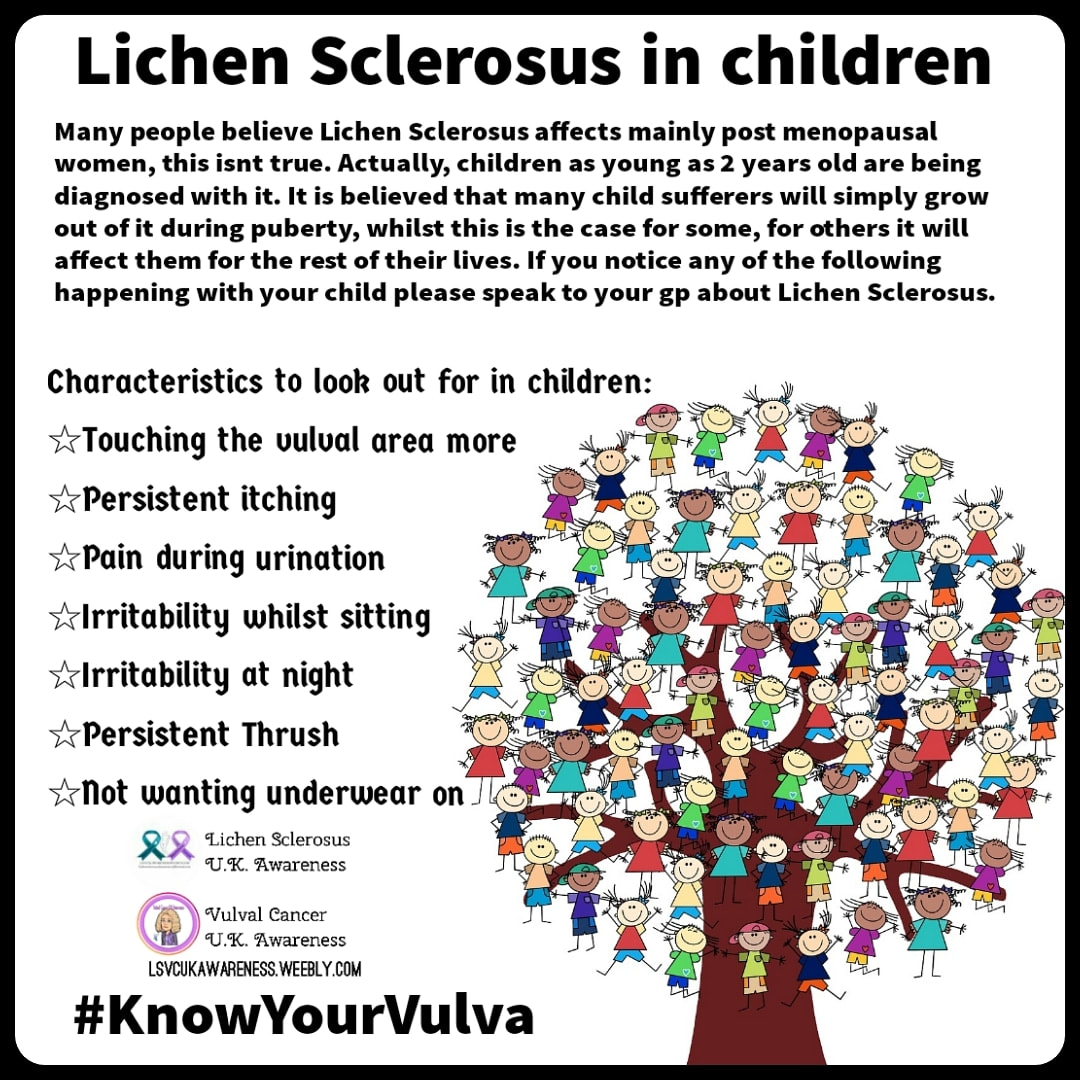



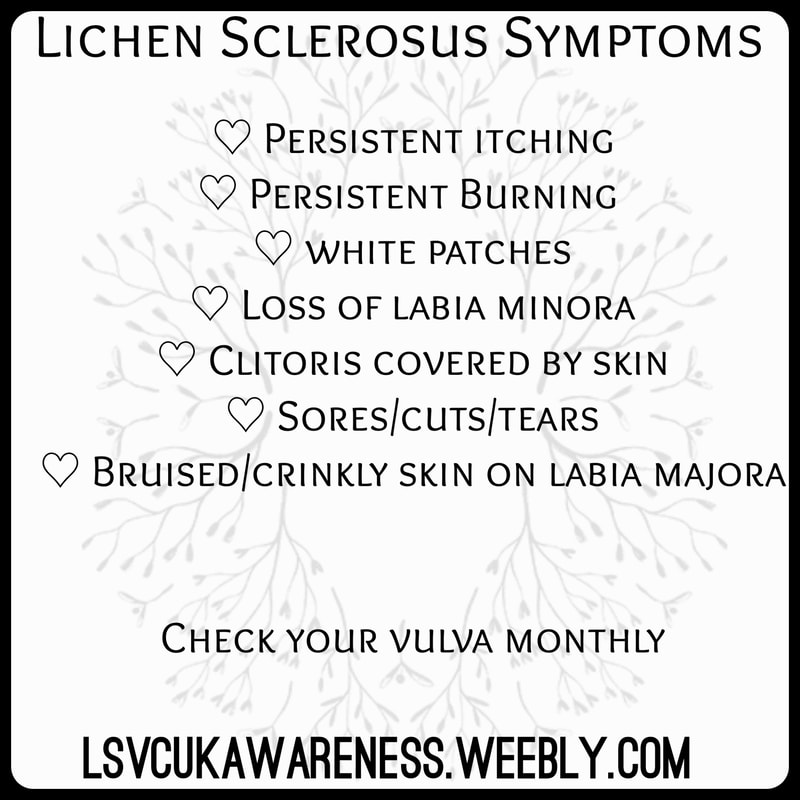

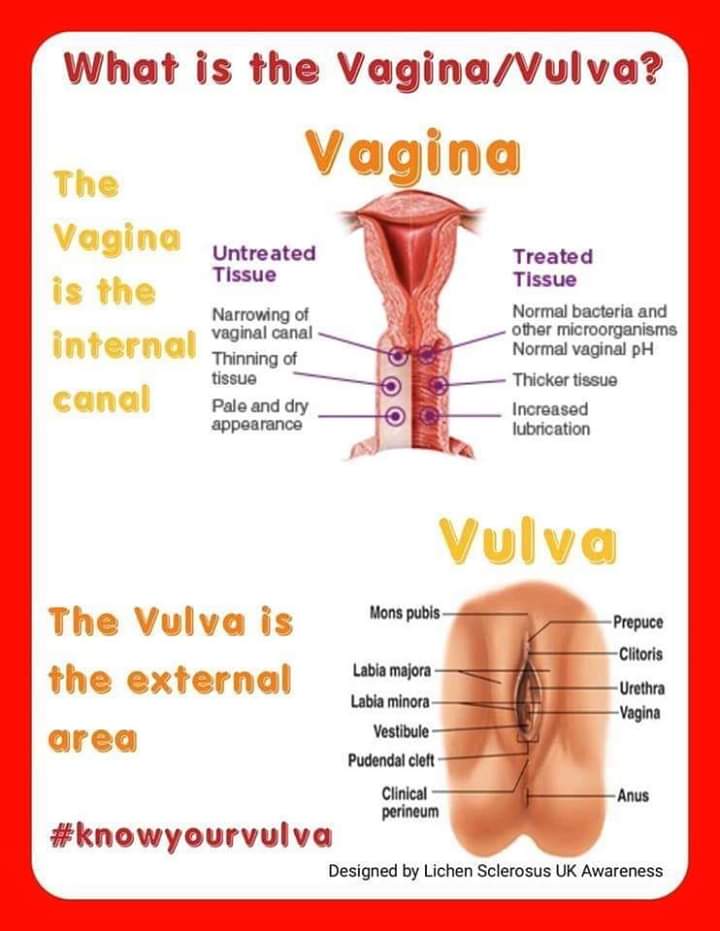
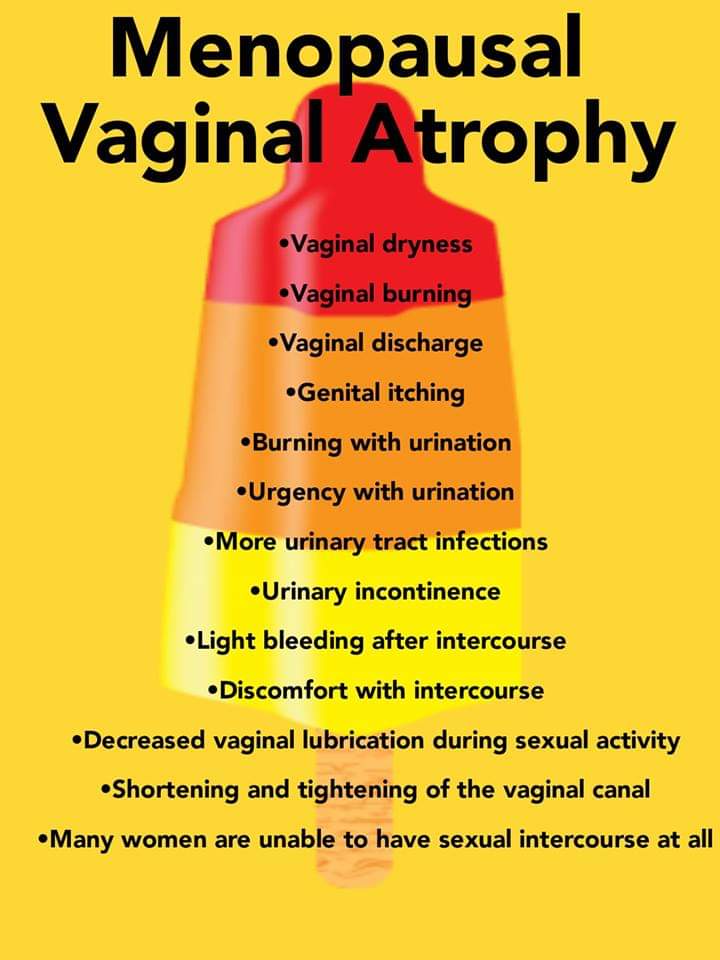
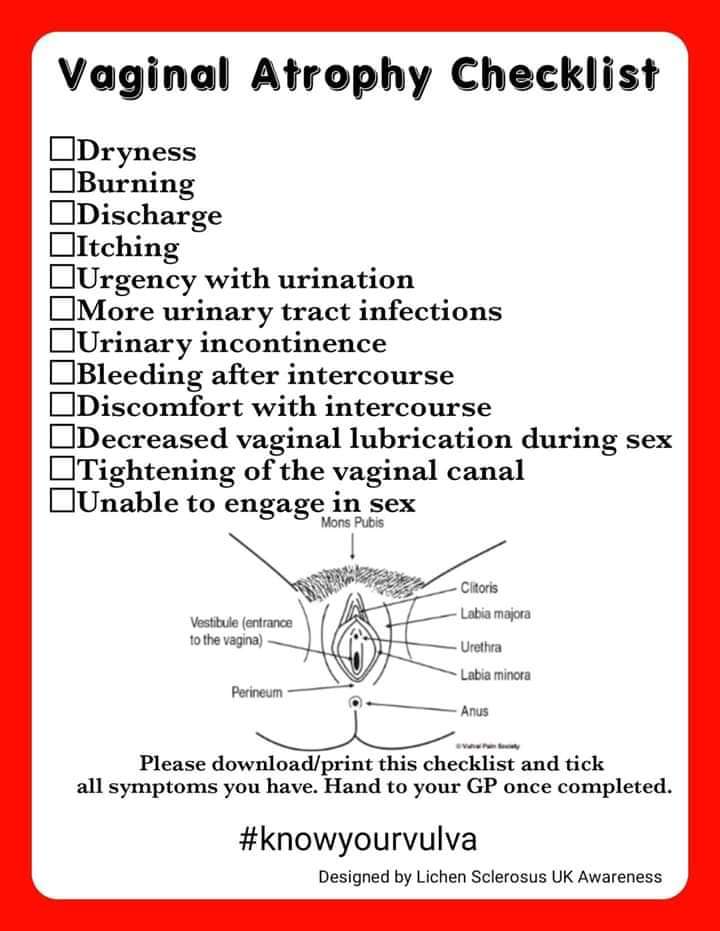

 RSS Feed
RSS Feed
